When the FDA slapped a black box warning on antidepressants for children and teens in 2005, the goal was simple: protect young lives. The message was clear - these medications might increase suicidal thoughts in kids. But what happened next wasn’t what anyone expected. Prescriptions dropped. Suicide attempts went up. And the very people meant to be protected ended up with less care, not more.
The Warning That Changed Everything
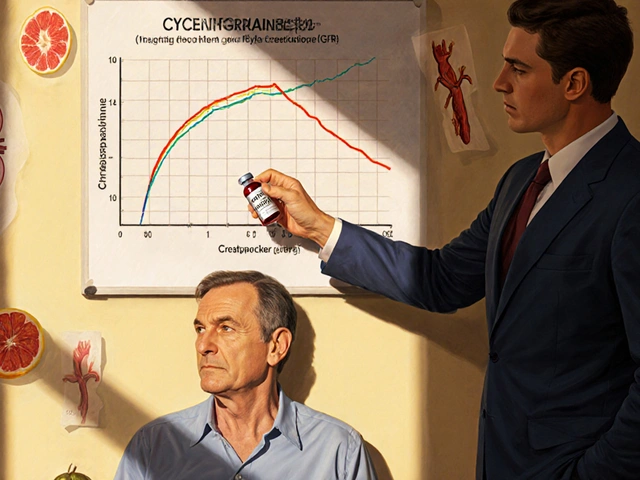
The FDA’s black box warning is the strongest safety alert they can issue. It’s bold, it’s framed in black, and it’s printed right on the label of every antidepressant prescribed to anyone under 25. The warning says these drugs may raise the risk of suicidal thinking and behavior in children and adolescents. It’s based on a review of 24 clinical trials involving over 4,400 young patients. The numbers showed a 2% increase in suicidal thoughts among those on antidepressants compared to those on placebos - from 2% to 4%. No actual suicides occurred in those trials, but the fear was enough to trigger a nationwide shift.The warning didn’t just apply to one drug. It covered every antidepressant on the market - SSRIs like Prozac and Zoloft, SNRIs, and others. Pharmacists were required to hand out MedGuides to patients and families. Doctors had to document consent forms. Monitoring rules were set: weekly check-ins for the first month, then every two weeks. It sounded reasonable. But real life doesn’t follow clinical trial protocols.
The Unintended Consequences
Within two years of the warning, antidepressant prescriptions for 10- to 19-year-olds dropped by 31%. That’s over a million fewer prescriptions annually. At the same time, diagnoses of depression in teens were rising. More kids were showing symptoms. More were struggling. But fewer were getting medication.The results were grim. Suicide rates among 10- to 19-year-olds jumped 75% between 2003 and 2007. Psychiatric drug poisonings - a proxy for suicide attempts - rose by 21.7% in the two years after the warning. When the FDA expanded the warning to include young adults up to age 24 in 2007, suicide attempt rates in that group climbed another 33.7%. Meanwhile, adults over 25 - not affected by the warning - saw no such spike.
Researchers at Harvard Pilgrim Health Care Institute looked at data from 1.1 million adolescents and 1.4 million young adults across 11 U.S. health plans. Their conclusion? The warning may have done more harm than good. The clinical trials showed a small rise in suicidal thoughts, but no increase in completed suicides. The real world, however, showed a sharp rise in actual harm - because treatment was avoided.
What Parents Are Really Thinking
On Reddit, parents post in threads like “Should I be worried about antidepressants for my teen?” The comments are split. Sixty-eight percent say they’re terrified of making things worse. One mother wrote, “I watched my daughter spiral for months because I was too scared to let her take the medicine the doctor recommended.”A 2021 survey by the National Alliance on Mental Illness found that 74% of parents delayed or refused antidepressants for their children because of the black box warning. The top reason? Fear that the drug would trigger suicidal behavior. But among those who did go ahead with treatment, 67% reported improvement. Many said the warning actually helped them stay alert - they checked in more often, noticed mood changes faster, and kept closer contact with their child’s doctor.
It’s not that parents don’t want help. They want to know the real trade-offs. They want to understand if the risk is worth it - not just a warning on a label, but a clear picture of what happens when you treat versus when you don’t.

Doctors Are Caught in the Middle
A 2019 survey of 1,200 child psychiatrists found that 87% had a harder time prescribing antidepressants after the warning. Parents demanded more time. More paperwork. More reassurance. The average consultation time jumped from 8 minutes to over 22 minutes just to explain the warning.Doctors are trained to weigh risks and benefits. But the black box warning doesn’t let them do that. It’s a one-size-fits-all alarm. It doesn’t say: “This risk is higher for kids with a history of self-harm.” Or “It’s lower for those with severe depression and no prior suicide attempts.” It just says: “Danger.”
And the monitoring rules? They’re nearly impossible to follow. A 2020 study found only 37% of youth patients got the recommended weekly check-ins. In rural areas, that number dropped to 22%. Many families live hours from a psychiatrist. Insurance doesn’t cover frequent visits. And even if they could, how many parents can take time off work every week for a 30-minute appointment?
The Global Picture
The U.S. isn’t alone in this debate - but it’s the only country with this exact warning. Health Canada has a similar alert, but it includes a line about balancing risks and benefits. The European Medicines Agency never issued a black box warning at all. And here’s the striking part: European countries didn’t see the same spike in youth suicides after 2005. In fact, their suicide rates stayed flat or even declined.That suggests the warning itself - not the drugs - might be part of the problem. When treatment drops, people don’t just get sicker. They get more isolated. More hopeless. More likely to act on thoughts they never got help for.

What’s Changing Now?
By 2023, the evidence was too strong to ignore. A major review in Health Affairs concluded the black box warning likely caused more harm than protection. The American College of Neuropsychopharmacology called for a reassessment. Eli Lilly and Pfizer asked the FDA to change the language. The FDA held a public meeting in September 2023 to review the data - but still hasn’t acted.Meanwhile, researchers at the National Institute of Mental Health are working on something better: risk prediction tools. Instead of warning everyone, they want to identify who’s truly at higher risk - based on genetics, trauma history, depression severity, and family support. That’s the future. Not a blanket warning. But personalized guidance.
The Bottom Line
Antidepressants aren’t magic. They don’t fix everything. But for many teens and young adults with severe depression, they’re the difference between surviving and not. The black box warning was meant to save lives. Instead, it may have taken them.The real risk isn’t the medication. It’s the silence that follows when families are too afraid to ask for help. It’s the months lost waiting for a doctor who’s overwhelmed. It’s the belief that doing nothing is safer than doing something.
If you’re a parent wondering whether to start your child on antidepressants, don’t let a warning on a label make the decision for you. Talk to a doctor who knows your child. Ask: What’s the risk of not treating? What does the evidence say for someone like my child? How will we monitor? What signs should I watch for?
The answer isn’t to avoid medication. It’s to use it wisely - with support, with monitoring, and with honesty about the risks and benefits. Because sometimes, the greatest danger isn’t the drug. It’s the fear that keeps you from using it.


james thomas
November 27 2025The FDA’s black box warning? Classic bureaucratic overreach. They didn’t just warn-they weaponized fear. Meanwhile, the real villains are the pharma reps pushing SSRIs like candy and the psychiatrists who outsource parenting to pills. This isn’t medicine. It’s a profit-driven distraction from systemic failures: broken schools, collapsing families, and zero mental health infrastructure. You think a pill fixes trauma? LOL. The suicide spike? That’s what happens when you take away the only tool kids had to cope while offering zero alternatives. The system didn’t fail. It was designed this way.