What Chronic Bronchitis Really Feels Like
You wake up every morning with a cough that won’t quit. It’s not just a tickle-it’s deep, wet, and exhausting. You bring up mucus, sometimes thick and yellow, sometimes clear but always too much. Walking to the mailbox leaves you gasping. Your chest feels tight, like someone’s squeezing it. And no matter how much you try to shake it off, this doesn’t go away after a week or two. It’s been months. Years, even.
This isn’t just a bad cold. This is chronic bronchitis. Doctors define it simply: a cough that brings up mucus for at least three months a year, for two years straight. It’s not something you grow out of. It’s not something you can ignore. And while it’s often grouped under COPD, it’s its own kind of struggle-one that changes how you breathe, move, and live.
Most people with this condition have smoked. About 75% of cases in the U.S. are tied to smoking or having smoked in the past. But not every smoker gets it. Only about 15% of people who smoke develop serious airflow problems. That means genetics, environment, and how long you’ve been exposed to irritants all play a role. Some people start noticing symptoms in their 40s. By 65, the numbers climb sharply.
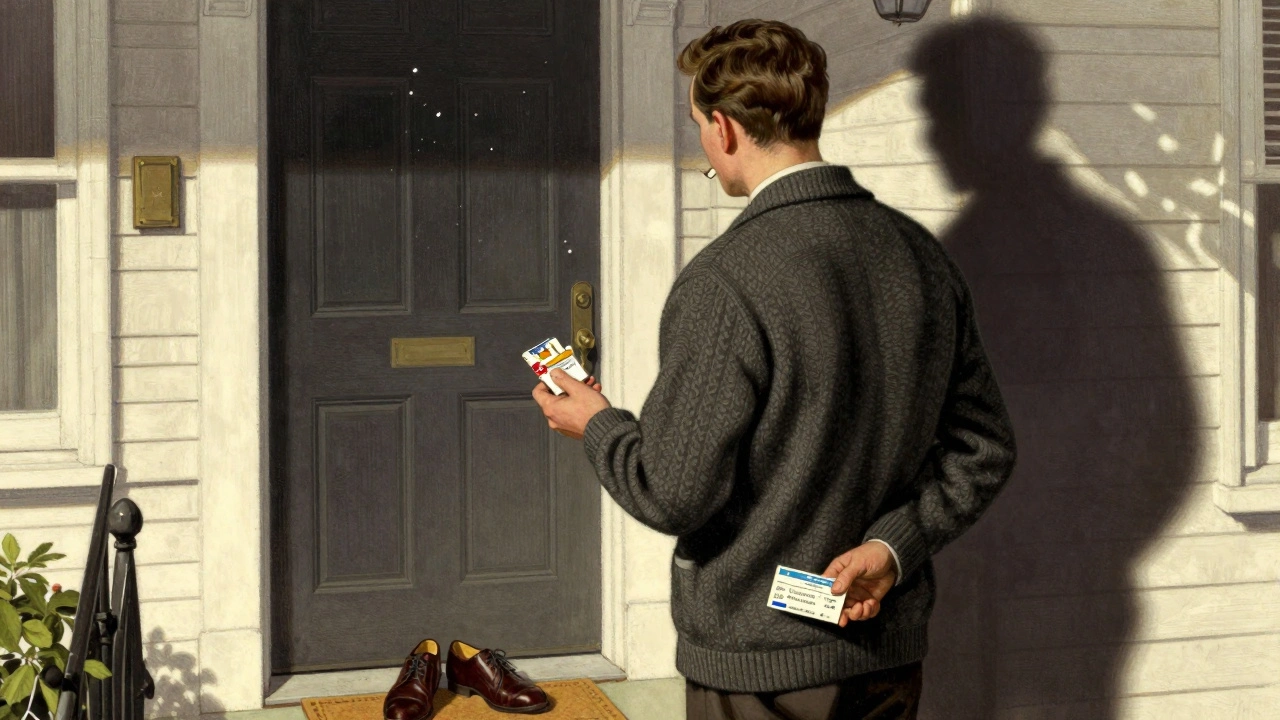
Why Smoking Is the Main Culprit-And Why Quitting Is the Only Real Cure
If you have chronic bronchitis, and you still smoke, nothing else you do will slow this disease as much as quitting. Not inhalers. Not pills. Not oxygen tanks. Nothing.
Studies show that people who quit smoking cut their disease progression in half. One major study found that those who stopped smoking had 60% slower lung function decline compared to those who kept smoking. That’s not a small difference. That’s the difference between needing oxygen at 65 or still walking without stopping at 75.
And it’s not just about your lungs. Smoking increases your risk of pneumonia, flu complications, and hospital visits by more than three times. Every cigarette you light up keeps your airways inflamed, makes mucus thicker, and weakens your body’s ability to fight off infections.
Quitting isn’t easy. Most people try multiple times before they succeed. But here’s the truth: people who get help-real help-quit at more than double the rate. If you try alone, your chance of success is about 7%. If you use a structured program with counseling and medication, that jumps to 45%.
That’s why doctors now say: quitting isn’t just part of treatment. It’s the treatment.
The Symptoms You Can’t Ignore
Chronic bronchitis doesn’t sneak up on you. It announces itself.
- A persistent cough-the kind that wakes you up at night or makes you miss work. This isn’t occasional. It’s daily, often for years.
- Excess mucus-you’re clearing your throat all day. You carry tissues. You avoid social situations because you’re afraid you’ll cough in public.
- Shortness of breath-even walking a few steps feels like climbing a hill. You stop mid-sentence to catch your breath.
- Chest tightness-like a band is wrapped around your ribs. It’s not heart pain, but it’s uncomfortable enough to make you anxious.
- Wheezing and fatigue-your lungs are working overtime, and your body is drained from the effort.
These aren’t just annoyances. They’re signs your airways are damaged. And the longer you wait to act, the worse it gets.

What Actually Works: Treatments That Change Outcomes
There’s no cure. But there are treatments that help you live better, longer.
Bronchodilators-these are inhalers that open your airways. Short-acting ones give quick relief when you’re struggling. Long-acting ones keep your lungs open all day. Many patients feel better within minutes.
Pulmonary rehabilitation-this isn’t just exercise. It’s a full program: breathing techniques, nutrition advice, education on your condition, and supervised physical training. People who complete it walk 78 meters farther on average and cut hospital visits by nearly 40%. And it’s not just for the severely ill. Even mild cases benefit.
Flu and pneumonia shots-annual flu vaccines reduce flare-ups by 42%. Pneumococcal vaccines cut pneumonia risk by two-thirds. These are simple, safe, and critical.
Oxygen therapy-if your blood oxygen drops below 88%, your body starts to suffer. Continuous oxygen for 15+ hours a day can increase your 5-year survival by 21%. It’s not a last resort. It’s a lifeline.
But not all treatments are created equal. Inhaled steroids? They help some people, but they raise your risk of bone fractures, high blood pressure, and diabetes. Many doctors now avoid them unless absolutely necessary.
The Hidden Battle: Adherence and Real-Life Challenges
Here’s the hard part: knowing what to do isn’t the same as doing it.
Only 54% of people take their medications exactly as prescribed. Why? Some forget. Others can’t afford them. Many just don’t know how to use their inhalers right. Studies show it takes nearly five sessions with a respiratory therapist for most people to master proper technique.
Oxygen therapy? Only 62% of patients use it as much as they should. Why? Because the tubes get tangled. Because it’s embarrassing to walk around with a tank. Because it’s heavy.
Exercise programs? Forty-one percent drop out within three months. It’s tiring. It’s discouraging. You don’t see instant results.
That’s why the best programs don’t just hand you a prescription. They walk with you. They check in. They adjust. They celebrate small wins-like walking to the end of the driveway without stopping.
What’s New in Treatment (And What’s Still the Same)
In 2023, the FDA approved a new drug called ensifentrine. It’s the first of its kind-a phosphodiesterase inhibitor that helps open airways and reduces mucus. In trials, it improved walking distance by 42 meters and cut flare-ups by 15%. It’s promising, but it’s not a magic bullet.
Researchers are also studying genes that affect mucus thickness. Soon, we might be able to match patients with the right mucolytic drugs based on their DNA. But that’s still in early testing.
Meanwhile, digital tools are helping. Inhalers with sensors track when you use them. Apps guide you through breathing exercises. Tele-rehab lets you do physical therapy from your living room.
But here’s the thing: none of this replaces quitting smoking. None of it replaces pulmonary rehab. None of it replaces staying up to date on vaccines.
The biggest breakthroughs aren’t new drugs. They’re better support systems. Better education. Better access to programs that help people stick with what works.
What You Can Do Today
Start with this: if you smoke, make quitting your #1 goal. Don’t wait for the next checkup. Call your doctor now. Ask about varenicline, nicotine patches, or counseling. Ask for a referral to a pulmonary rehab program-even if you think you’re not sick enough.
If you don’t smoke but have a persistent cough and mucus, get tested. Many people assume it’s just "smoker’s cough" or "aging." It might be chronic bronchitis. Early diagnosis means better outcomes.
And if you’re already managing this condition: don’t give up. Small steps add up. One more walk. One more day without smoking. One more vaccine. One more inhaler session done right.
Your lungs are still working. They’re still fighting. Help them.
Is chronic bronchitis the same as COPD?
Chronic bronchitis is one type of COPD, along with emphysema. COPD is the umbrella term for lung diseases that cause airflow blockage. Chronic bronchitis specifically means long-term inflammation of the bronchial tubes, leading to mucus buildup and cough. Not everyone with COPD has chronic bronchitis, but most people with chronic bronchitis have COPD.
Can you get chronic bronchitis if you never smoked?
Yes, but it’s less common. About 22% of people with chronic bronchitis have never smoked. Other causes include long-term exposure to air pollution, dust, chemical fumes, or secondhand smoke. A rare genetic condition called alpha-1 antitrypsin deficiency can also cause it, but this accounts for only about 2% of cases.
Do inhalers cure chronic bronchitis?
No. Inhalers help manage symptoms by opening airways and reducing coughing, but they don’t reverse lung damage. The only way to slow the disease is to stop smoking and protect your lungs from further harm. Inhalers are tools for daily comfort, not cures.
How long does it take to see results after quitting smoking?
Within weeks, your lungs start to clear mucus and breathing improves. After six months, many people notice less coughing and more energy. After one year, lung function stops declining as fast. After five years, the risk of serious complications drops significantly. The damage doesn’t disappear, but your body starts to heal.
Is pulmonary rehab worth the effort?
Yes, especially if you’re feeling limited by your symptoms. People who complete pulmonary rehab report better breathing, more strength, and fewer hospital stays. Studies show it improves daily life more than any single medication. It’s not a quick fix-but it’s one of the most effective things you can do.




Kay Jolie
December 5 2025Okay but let’s be real-this post reads like a pharmaceutical whitepaper written by someone who’s never actually had to cough up a lung before. Bronchodilators? Pulmonary rehab? Please. The only thing that works is quitting smoking. Everything else is just expensive placebo theater with a side of insurance billing codes. I’ve seen patients on five different inhalers still wheezing like a broken accordion because they refuse to let go of the habit. It’s not about meds-it’s about willpower. Or lack thereof.