Cyclosporine Target Level Calculator
Cyclosporine Monitoring Guide
Find your target cyclosporine level range based on your transplant type and time since surgery. Always consult your healthcare team for personal medical advice.
When you take cyclosporine after a kidney, heart, or liver transplant, it’s not just about preventing rejection. It’s about staying alive without wrecking your kidneys. Cyclosporine is powerful - but it’s also one of the most dangerous drugs you can take if you don’t watch it closely. About cyclosporine nephrotoxicity affects 25% to 75% of transplant patients. That’s not rare. That’s common. And it’s not just a side effect - it’s the #1 reason transplanted kidneys fail over time.
Why Cyclosporine Hits the Kidneys So Hard
Cyclosporine doesn’t attack the kidney like a toxin. It strangles it. The drug tightens blood vessels inside the kidney, reducing blood flow. That’s called renal vasoconstriction. Less blood means less filtration. Creatinine rises. GFR drops. Over time, this leads to scarring - arteriolar hyalinosis, tubular vacuolization, interstitial fibrosis. These aren’t just lab terms. They’re permanent damage.
And here’s the kicker: you won’t feel it until it’s advanced. No pain. No swelling. Just a slow, silent decline in kidney function. That’s why monitoring isn’t optional. It’s survival.
What Levels Are Safe? It Depends
There’s no single ‘good’ cyclosporine level. It changes over time. It changes by organ. It changes by your body’s genetics.
- Kidney transplant: First week? 200-400 ng/mL. After six months? Drop to 100-150 ng/mL. After a year? 75-160 ng/mL.
- Heart or liver transplant: First six months: 250-350 ng/mL. After that: 100-200 ng/mL.
But those are old targets. Newer data from 2023 shows many centers now use C2 monitoring - measuring blood levels two hours after your dose. Why? Because C2 levels correlate better with how much drug your body actually absorbed over the whole day. Studies show switching to C2 cuts rejection rates by nearly 20% and reduces kidney damage by over 22%.
And now, genetics matter. If you’re an ‘extensive metabolizer’ of CYP3A5 - about 1 in 3 people - your body clears cyclosporine faster. You may need 30-40% more than someone who metabolizes it slowly. No one checks this unless you ask. You should.
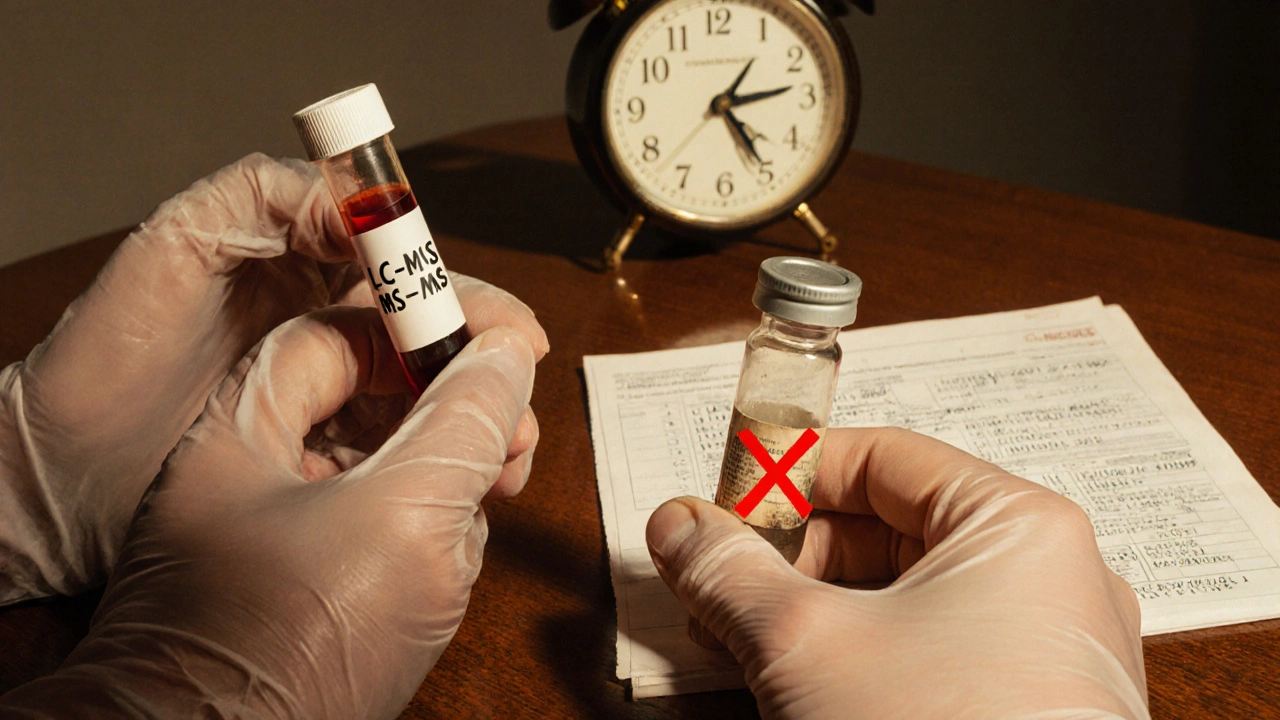
How Do They Measure Cyclosporine? Not All Tests Are Equal
There are three ways labs test cyclosporine levels. Only one is truly accurate.
| Method | Accuracy | Turnaround Time | Cost per Test | Used By |
|---|---|---|---|---|
| LC-MS/MS (Liquid Chromatography-Tandem Mass Spectrometry) | 99.2% specific | 4-6 hours | $40-$60 | 92% of U.S. transplant centers (2021) |
| HPLC (High-Performance Liquid Chromatography) | 95-98% specific | 6-8 hours | $35-$50 | Declining use |
| Non-isotopic Immunoassay | 85-90% specific (cross-reacts with metabolites) | 2-4 hours | $15-$25 | Still common in smaller labs |
Immunoassays are cheap and fast - but they often give falsely high readings because they can’t tell the difference between cyclosporine and its metabolites. That means doctors might lower your dose when you actually need more. That’s dangerous.
LC-MS/MS is the new gold standard. It’s precise. It’s specific. It’s expensive. But if your lab still uses immunoassays, ask why. Your kidney health depends on this.
What Else Needs Monitoring? Beyond Just Cyclosporine Levels
Looking at cyclosporine alone is like checking only the gas gauge and ignoring the engine temperature. You need the full picture.
- Serum creatinine: Keep it under 1.5 mg/dL. Rising levels mean your kidneys are struggling.
- BUN-to-creatinine ratio: Should be under 20:1. Higher ratios suggest dehydration or reduced kidney blood flow.
- Magnesium: Cyclosporine causes magnesium loss. Normal range is 1.7-2.2 mg/dL. Low magnesium = muscle cramps, irregular heartbeat, worse kidney damage.
- Blood pressure: Target is below 130/80 mmHg. High BP speeds up kidney scarring.
- Drug interactions: Ketoconazole, erythromycin, grapefruit juice - they can spike cyclosporine levels by 30-50%. Rifampin, phenytoin, St. John’s wort - they can crash levels by 40-60%. Tell every doctor you see you’re on cyclosporine. Every time.
And don’t forget: it takes 4-6 weeks for your body to reach steady state after a dose change. If you get a new prescription or your dose is adjusted, don’t panic if your labs look off in the first week. Wait. Recheck. Don’t overreact.
How Often Should You Get Tested?
There’s no one-size-fits-all schedule. But here’s what most top transplant centers follow:
- First month: Twice a week
- Months 2-6: Once a week
- Months 7-12: Every two weeks
- After one year: Monthly or every six weeks - if everything’s stable
But if your creatinine rises, your blood pressure spikes, or you start a new medication - go back to weekly testing. No exceptions.
And here’s a critical detail: blood must be drawn in EDTA tubes - not regular serum tubes. Serum tubes can cause falsely high readings by 15-20%. If your lab uses the wrong tubes, ask them to switch. This is a known error. Fixable.
Can the Damage Be Reversed?
Yes - if caught early.
Studies from the 1980s still hold up: if you reduce cyclosporine dose as soon as kidney function starts to decline, about 60-70% of patients see improvement within three months. The scarring stops. Blood flow improves. Creatinine drops.
But wait too long? The damage becomes permanent. That’s why early detection isn’t just helpful - it’s everything.
What’s Next? The Future of Monitoring
Artificial intelligence is coming. Trials are testing algorithms that use 17 different factors - your weight, age, genetics, diet, other meds, time since transplant - to predict the perfect cyclosporine dose. Early results show 89.7% accuracy. That could mean fewer blood draws and fewer mistakes.
Point-of-care devices are in Phase 3 trials. Imagine getting your cyclosporine level checked in 15 minutes with a finger-prick blood sample - right in the clinic. FDA approval is expected in late 2025.
But until then? You still need to be your own advocate. Know your numbers. Know your labs. Ask questions. Don’t assume your doctor knows everything. Cyclosporine is old. But the rules for using it safely are still evolving.
What If You Can’t Tolerate Cyclosporine?
Some people can’t. Their kidneys keep failing. Their blood pressure won’t budge. Their levels stay too high even on low doses.
That’s when doctors switch to tacrolimus - another calcineurin inhibitor, but with better kidney safety in most patients. Or mycophenolate, sirolimus, or belatacept. Each has trade-offs. But cyclosporine isn’t the only option. If you’re struggling, ask: Is there a better drug for me?
Don’t wait for your kidney to fail before you ask.
How do I know if cyclosporine is hurting my kidneys?
You won’t feel it. That’s the danger. Signs are only visible through lab tests: rising creatinine, falling GFR, high blood pressure, low magnesium. If your creatinine increases by more than 25% from baseline over a few weeks, that’s a red flag. Don’t wait for symptoms - monitor regularly.
Can I take cyclosporine with grapefruit juice?
No. Grapefruit juice blocks the enzyme that breaks down cyclosporine. This can cause levels to spike by 30-50%, increasing kidney damage risk. Avoid it completely. Same goes for pomegranate, Seville oranges, and certain supplements like St. John’s wort.
Why do some labs use different tests for cyclosporine?
Cost and convenience. Immunoassays are cheaper and faster, but they overestimate levels because they can’t tell cyclosporine from its metabolites. LC-MS/MS is more accurate but expensive. If your lab uses immunoassays and your levels seem too high, ask if they can switch to LC-MS/MS - your kidney health depends on accurate numbers.
Is C2 monitoring better than trough (C0) levels?
Yes, for most patients. C2 (2-hour post-dose) levels better reflect how much drug your body absorbed overall. Studies show C2 monitoring reduces rejection by nearly 20% and cuts nephrotoxicity by over 22% compared to just checking trough levels. Ask your transplant team if they use C2 - if not, ask why.
How long does it take for cyclosporine levels to stabilize after a dose change?
It takes 4 to 6 weeks. Your body doesn’t adjust instantly. If you change your dose, don’t retest after a few days - wait at least four weeks. Otherwise, you’ll see misleading numbers and might make unnecessary adjustments.
Can I stop cyclosporine if my kidney function improves?
Never stop without your transplant team’s guidance. Stopping cyclosporine suddenly can trigger acute rejection - which can destroy your transplant in days. If your kidneys are improving, your doctor may reduce the dose, but never stop it on your own.
Managing cyclosporine isn’t just about following a schedule. It’s about understanding your body, asking the right questions, and demanding accurate testing. Your kidney is your lifeline. Treat it that way.



Joe Durham
November 19 2025Man, this post is a lifesaver. I’ve been on cyclosporine for 3 years post-kidney transplant and no one ever explained C2 monitoring to me until now. My last three labs were all over the place, and my doc just kept saying ‘it’s fine.’ Turns out they were using immunoassays. I just requested LC-MS/MS last week - waiting on results, but finally feel like I’m being heard.
Thanks for the breakdown on magnesium too. I’ve been cramping like crazy and thought it was just aging. Turns out I’m at 1.4 mg/dL. Started supplements yesterday. Fingers crossed.