When you pick up a prescription for a generic drug, you might be handed a different pill than the one you got last month. Same name, same dose, same color-but a different manufacturer. It’s not a mistake. It’s normal. And it’s happening more than ever. In 2022, 90% of all prescriptions filled in the U.S. were for generic drugs. That’s over 5.8 billion prescriptions. The reason? Cost. Generics cost 80-85% less than brand-name versions, saving the healthcare system nearly $373 billion that year.
But here’s the question most people don’t ask: Are all generics the same? If you’re taking a medication for heart failure, thyroid disease, or epilepsy, the answer isn’t as simple as yes or no. Switching between different generic versions can matter-especially if your condition needs very precise drug levels.
What Makes a Generic Drug “Approved”?
The U.S. Food and Drug Administration (FDA) doesn’t just let any company make a copy of a brand-name drug. Before a generic can be sold, it must prove it works the same way in your body. This isn’t about looking alike or tasting the same. It’s about science.
To get FDA approval, a generic drug must match the brand in four key ways:
- Same active ingredient
- Same strength
- Same dosage form (pill, liquid, injection, etc.)
- Same route of administration (taken by mouth, injected, applied to skin, etc.)
But the real test is bioequivalence. That means the generic must deliver the active ingredient into your bloodstream at a rate and amount very close to the brand-name drug. The FDA requires that the generic’s absorption falls within 80% to 125% of the brand’s levels, measured by two key metrics: AUC (total exposure over time) and Cmax (peak concentration).
Let’s be clear: this doesn’t mean a generic could have 20% less drug in it. That’s a common myth. The 80-125% range is a statistical confidence interval. In practice, most approved generics are within 3-5% of the brand’s performance. A 2015 FDA study found that, on average, the difference between generics and brand-name drugs was just 3.5% in how much of the drug entered the bloodstream.
Not All Generics Are Created Equal
Even though every approved generic meets FDA standards, not all are equally reliable when switching back and forth. The FDA assigns a therapeutic equivalence (TE) code to each generic in its Orange Book, a public database that lists all approved drugs and their ratings.
Here’s what those codes mean:
- AB: Therapeutically equivalent. These generics have been proven bioequivalent to the brand and to each other. You can switch between AB-rated generics without expected changes in effect.
- B: Not rated as equivalent. These may meet basic requirements but have documented differences in how they’re absorbed. They’re approved for initial use, but switching from a brand to a B-rated generic-or between two B-rated generics-could cause issues.
For most medications-like antibiotics, blood pressure pills, or antidepressants-AB-rated generics are perfectly safe to swap. But for drugs with a narrow therapeutic index (NTI), even tiny changes in blood levels can be dangerous.
Which Medications Need Extra Caution?
NTI drugs are those where the difference between a helpful dose and a harmful one is very small. Switching generics here isn’t just about cost-it’s about safety.
Examples include:
- Levothyroxine (for hypothyroidism): Even a 10% change in absorption can cause symptoms like fatigue, weight gain, or heart palpitations. The FDA issued warning letters to multiple manufacturers in 2021 over inconsistent bioequivalence. Since then, testing requirements have tightened.
- Digoxin (for heart failure): Small changes in blood levels can trigger dangerous heart rhythms. The UCSF Medical Center advises sticking with one manufacturer once you’re stable.
- Warfarin (a blood thinner): A slight increase in concentration can cause bleeding; a drop can cause clots. Patients on warfarin are often advised to stay on the same generic brand.
- Phenytoin (for seizures): Fluctuations can lead to breakthrough seizures.
A 2017 study in Circulation: Cardiovascular Quality and Outcomes looked at generic versions of the blood pressure drug candesartan. It found that patients switching to a new generic had a higher rate of adverse events in the first month-though the risk dropped after that. This suggests that while most people adapt, some don’t.

How to Make the Right Choice
So how do you pick the right generic? Here’s a practical guide:
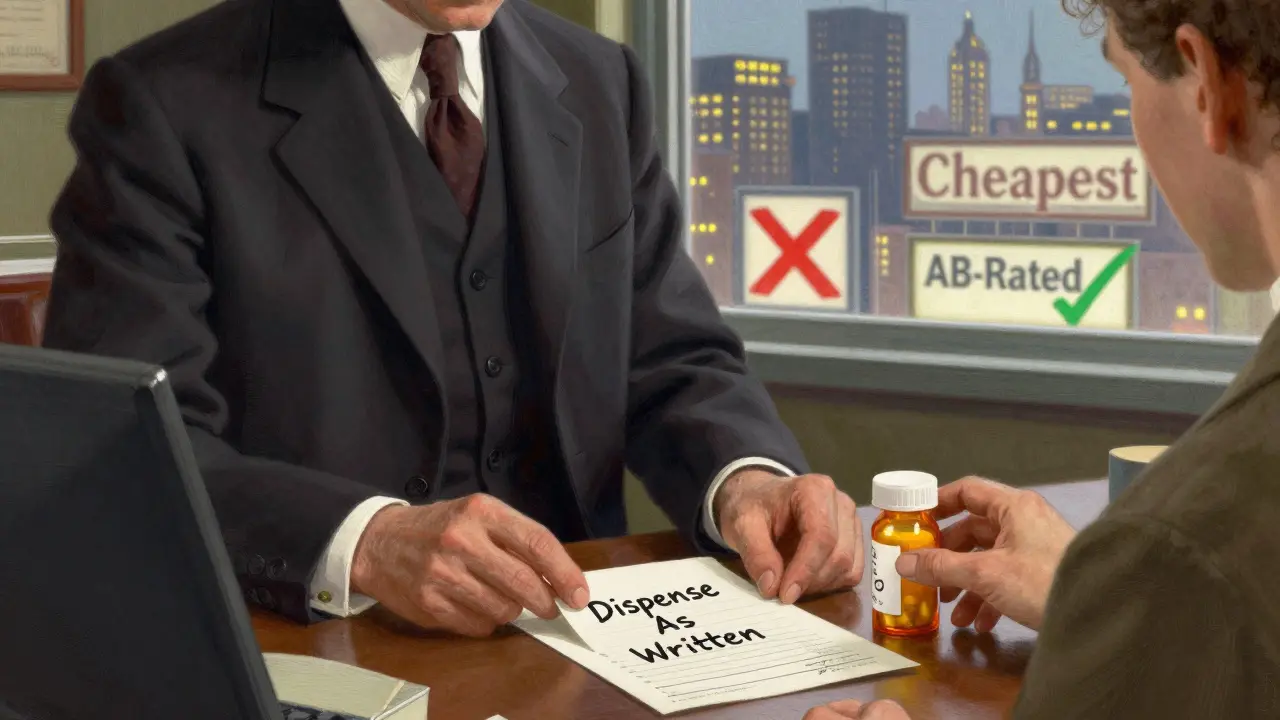
- Check the TE code. Ask your pharmacist for the FDA’s therapeutic equivalence rating. If it’s AB, you’re in the safest group. If it’s B, ask why it’s being prescribed and whether switching is necessary.
- Don’t switch unless you have to. If you’re stable on a brand-name drug, there’s no benefit to switching to a generic unless cost is a barrier. If you’re already on a generic, stick with the same manufacturer. Frequent switching-even between AB-rated generics-can disrupt your body’s balance, especially with NTI drugs.
- Use the same pharmacy. Pharmacists keep records of which manufacturer’s version you’ve been taking. If you switch pharmacies, you might get a different generic without realizing it. Tell your pharmacist you prefer consistency.
- Monitor your symptoms. If you start feeling different after a switch-more tired, dizzy, anxious, or experiencing new side effects-don’t ignore it. Contact your doctor. It could be the generic.
- Ask for a specific brand. Your prescriber can write “dispense as written” on your prescription. That stops automatic substitution. This is especially important if you’ve had problems with generics before.
Why Do So Many Generics Exist?
There’s a reason you see five different versions of the same pill. After a brand-name drug’s patent expires, dozens of companies can apply to make generics. As of October 2023, the FDA listed over 14,000 generic products for just 2,745 active ingredients. That’s an average of 5.25 manufacturers per drug.
More competition means lower prices. But it also means more confusion. In 2022, 96% of generic drugs had three or more makers competing. That’s great for your wallet-but not always great for your health if you’re switching back and forth.
Some states have rules to help. As of January 2023, 28 states require pharmacists to notify your doctor if they switch you to a different manufacturer’s generic. That’s not universal, though. So don’t assume you’ll be told.
What’s Changing in 2025?
The FDA is tightening rules for complex generics-like extended-release pills, inhalers, and topical creams-because they’re harder to copy accurately. In 2022, new requirements kicked in under GDUFA III, forcing manufacturers to prove bioequivalence with stricter testing.
In 2021, the FDA flagged multiple generic levothyroxine products for inconsistent performance. Since then, testing protocols have been updated. That means newer versions of this drug are more reliable-but older ones may still be on shelves.
There’s also a proposed law, the Generic Drug Labeling Act, that would require each generic manufacturer to have a unique National Drug Code (NDC). Right now, all versions of, say, metformin 500mg look the same on the label. If the law passes, you’ll be able to tell exactly which company made your pill-making it easier to track side effects and avoid bad batches.
Bottom Line: When to Stick, When to Switch
For most people, generics are safe, effective, and the smart financial choice. But for those on critical medications, consistency matters more than savings.
Here’s what to do:
- If you’re starting a new medication: Choose an AB-rated generic. It’s cheaper and just as effective.
- If you’re already stable on a brand or generic: Don’t switch unless your doctor or pharmacist recommends it. Keep using the same version.
- If you’re on a narrow therapeutic index drug: Ask your doctor to write “dispense as written” and stick with one manufacturer. Don’t let your pharmacy switch you without telling you.
- If you notice changes after a switch: Call your doctor. Don’t wait. Your body might be reacting to a different formulation.
Generics saved billions. But they’re not all interchangeable. The difference between a good choice and a risky one isn’t always obvious. The key is knowing your drug, asking questions, and staying consistent.
Are all generic medications the same as the brand-name version?
By law, generics must have the same active ingredient, strength, dosage form, and route of administration as the brand. They must also be bioequivalent-meaning they deliver the drug into your bloodstream at nearly the same rate and amount. The FDA requires this before approval. However, inactive ingredients (like fillers or coatings) can differ, and in rare cases, these differences can affect how the drug is absorbed-especially with complex or narrow therapeutic index drugs.
Can I safely switch between different generic versions of the same drug?
For most medications, yes-especially if they’re rated AB by the FDA. But for drugs like levothyroxine, digoxin, warfarin, or phenytoin, switching between generics-even AB-rated ones-can cause changes in blood levels that affect your health. The safest approach is to stick with one manufacturer once you’ve found a version that works for you.
What does an AB rating mean on the FDA Orange Book?
An AB rating means the generic drug has been shown to be therapeutically equivalent to the brand-name drug. It has the same active ingredient, strength, and bioequivalence profile. AB-rated generics can be substituted for the brand or for each other without expected changes in safety or effectiveness. This is the highest rating the FDA gives.
Why do some pharmacists switch my generic without asking?
In most states, pharmacists are allowed to substitute a generic for a brand-name drug unless the prescription says “dispense as written.” Many states also allow substitution between different generics. This is done to save money. But in 28 states, pharmacists must notify your doctor if they switch you to a different manufacturer. Always check your prescription label and ask if your medication changed.
How do I find out which generic manufacturer I’m taking?
Look at the pill itself. Generic pills often have an imprint code (letters or numbers) that identifies the manufacturer. You can search this code on websites like Drugs.com or use the FDA’s Orange Book to look up the NDC number on your prescription label. Your pharmacist can also tell you the manufacturer and whether it’s AB-rated.
Should I always choose the cheapest generic?
For most medications, yes-especially if it’s AB-rated. But for drugs where small changes in blood levels matter (like thyroid, heart, or seizure meds), the cheapest option isn’t always the safest. If you’re stable on a specific version, paying a little more to stay on it may be worth avoiding potential side effects or hospital visits. Talk to your doctor or pharmacist about your options.
What to Do Next
If you’re on a medication that’s critical to your health, take five minutes today to check:
- What’s the TE code for your generic? (Ask your pharmacist)
- Are you on the same manufacturer as last time?
- Have you noticed any changes in how you feel since your last refill?
If you’re unsure, don’t guess. Call your doctor. Bring your pill bottle. Ask: “Is this the right version for me?” It’s not about being difficult-it’s about being safe.



Katherine Blumhardt
December 26 2025So like... I just got my levothyroxine switched again and now I feel like a zombie? 🤷♀️ no cap my heart’s racing and I’m sweating through my hoodie at 7am. pharmacist said ‘it’s the same thing’ but bro it’s not. I swear this one tastes weird too.