It’s one of the most common and frustrating questions patients face: are these symptoms from my illness, or from the medicine I’m taking to treat it? You start a new pill for high blood pressure, and suddenly you’re dizzy. You begin an antidepressant, and now you can’t sleep. You’re on a statin for cholesterol, and your muscles ache. Is this your condition getting worse-or is it the drug?
The truth is, you’re not alone. About 40% of people with chronic conditions end up confused about whether what they’re feeling is the disease or the treatment. And when you mix them up, you risk taking more pills, getting unnecessary tests, or stopping something that’s actually helping you. This isn’t just inconvenient-it’s dangerous.
Know the Difference: Symptoms vs. Side Effects
Disease symptoms are what your body shows because of the illness itself. For example, if you have depression, you might feel tired, lose interest in things, have trouble concentrating, or sleep too much or too little. These are classic signs of the condition, not the medicine.
Side effects, on the other hand, are unintended reactions to the drug. They’re not part of your disease. They’re your body’s response to the chemical in the pill. The World Health Organization defines them clearly: side effects happen when you take a medication at a normal dose, and the reaction isn’t the one you’re trying to achieve.
Think of it this way: if you’re taking lisinopril for blood pressure and you develop a dry, nagging cough, that’s a known side effect-not a sign your lungs are failing. If you’re on sertraline for anxiety and you lose interest in sex, that’s a common side effect-not a sign your depression is deepening.
Timing Is Everything
One of the clearest ways to tell the difference is when the symptom started.
Side effects usually show up shortly after you begin a new medication-or after a dose change. Most common ones appear within 1 to 4 weeks. For example:
- Nausea from an SSRI? Often hits within days.
- Drowsiness from an antihistamine? Right after you take it.
- Weight gain from an antipsychotic? Usually noticeable after 6 to 12 weeks.
Disease symptoms, however, tend to follow their own pattern. Depression doesn’t suddenly get worse because you took a pill on Tuesday. Arthritis pain doesn’t flare up the day after you start a new blood pressure med. If your symptoms line up with when you started or changed your medication, that’s a strong clue it’s a side effect.
Dose Matters
Another big clue? Does the symptom get worse when you take more of the drug-and better when you take less?
Seventy percent of side effects are dose-dependent. That means if you double your dose and your headache doubles, it’s likely the medication. If you cut your dose in half and your dizziness fades, that’s another sign.
Disease symptoms don’t usually respond to dose changes. Your joint pain from rheumatoid arthritis won’t suddenly improve just because you took half your usual dose of methotrexate. It might get worse if you skip it entirely-but not because the dose was too high.
Common Side Effects to Watch For
Some side effects are so common they’re practically expected:
- Nausea (25-30% of people starting new meds)
- Constipation (15-20%)
- Dry mouth (12-18%)
- Drowsiness (10-15%)
- Headache (7-10%)
- Rash (8-12%)
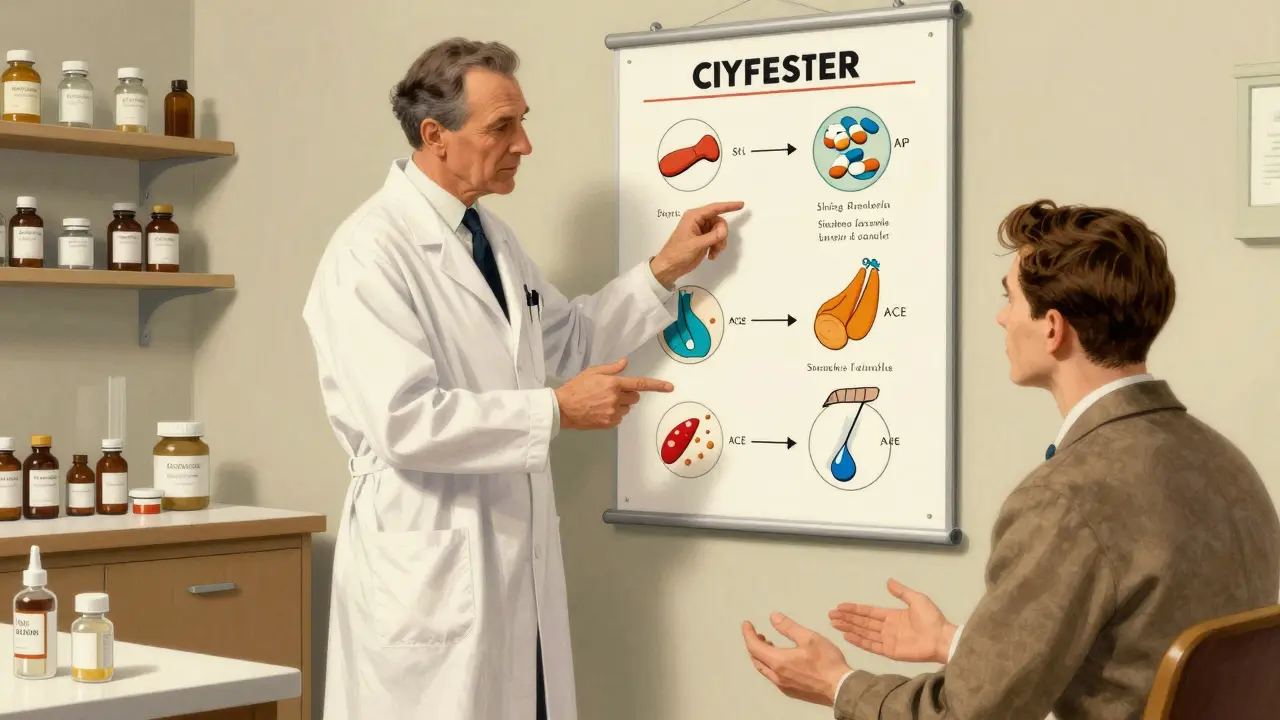
Some drugs have signature side effects:
- ACE inhibitors (like lisinopril) → persistent dry cough
- SSRIs (like sertraline, fluoxetine) → sexual dysfunction, insomnia, nausea
- Antipsychotics (like olanzapine) → weight gain, increased appetite
- Statins (like atorvastatin) → muscle aches, fatigue
- Anticholinergics (like oxybutynin) → confusion, memory issues (especially in older adults)
These aren’t rare. They’re well-documented. If you’re on one of these drugs and feel one of these things, it’s worth asking: could this be the pill?
What About Allergic Reactions?
Don’t confuse side effects with allergies. Allergic reactions are different. They’re not predictable. They’re not dose-dependent. And they can be serious.
Signs of an allergic reaction:
- Hives or itchy rash
- Swelling of the face, lips, or tongue
- Difficulty breathing
- Wheezing or tight chest
If you have any of these, stop the medication and get help immediately. Allergies happen fast-within minutes to hours-and can be life-threatening. Side effects? They usually build slowly.
The ‘Dechallenge-Rechallenge’ Trick (Under Supervision)
Doctors use a method called dechallenge-rechallenge to confirm side effects. Here’s how it works:
- Dechallenge: You stop the medication (only under your doctor’s guidance).
- Wait: See if the symptom improves over days or weeks.
- Rechallenge: You restart the medication and watch if the symptom comes back.
If the symptom disappears when you stop the drug and returns when you restart it, that’s a strong signal it’s a side effect. This method is about 85% accurate.
But don’t try this on your own. Stopping some meds suddenly can be dangerous-like antidepressants or blood pressure drugs. Always work with your doctor.
Keep a Symptom Journal
One of the most powerful tools you have is a simple notebook or app.
Write down:
- What medicine you took and when
- What dose
- What symptom you felt
- When it started
- How bad it was (1 to 10)
- How long it lasted
- Any other triggers (stress, food, sleep)
Studies show patients who keep these journals improve diagnostic accuracy by 41%. You’ll spot patterns your doctor might miss. For example, if your headache only happens after you take your afternoon pill-but not your morning one-you’ve found a clue.
Apps like Medisafe or MyTherapy can automate this. They send reminders and let you log symptoms right after you take your meds.
Don’t Ignore Polypharmacy
If you’re taking five or more medications, your risk of side effects jumps. One in three people on multiple drugs have symptoms that look like disease progression-but are actually drug interactions.
For example: you’re on a blood thinner, a diuretic, and an antidepressant. The diuretic makes you lose potassium. The antidepressant slows how your body processes the blood thinner. Now you’re dizzy and fatigued. Is it your heart? Your depression? Or a dangerous interaction?
Ask your pharmacist to do a full med review. Many pharmacies offer this for free. They can spot hidden conflicts your doctor might overlook.
When to Worry
Not every side effect needs panic. Some fade after a few weeks as your body adjusts. Nausea from an SSRI? Often gone in 2-3 weeks. Drowsiness from a sleep aid? Usually improves after a few days.
But call your doctor right away if you have:
- Sudden confusion or memory loss (could be anticholinergic side effects)
- Unexplained bruising or bleeding
- Severe muscle pain or weakness (possible statin myopathy)
- Swelling in your ankles or sudden weight gain (could be heart or kidney issue from meds)
- Thoughts of self-harm or worsening depression after starting a new drug
These aren’t typical side effects. They’re red flags.
What Your Doctor Should Be Doing
Good prescribers don’t just hand you a script. They tell you what to expect. The FDA now requires all patient medication guides to include a section on ‘symptoms vs. side effects.’ Your doctor should tell you:
- Which side effects are common and temporary
- Which ones need immediate attention
- When to expect them to start and stop
If they didn’t, ask. Say: ‘What side effects should I watch for? How do I know if this is the medicine or my condition?’
Pharmacists are your allies here too. They know the fine print. Ask them: ‘Is this symptom on the list of known side effects?’
Real Stories, Real Confusion
One woman on Reddit thought her SSRI was making her depression worse. She was exhausted, couldn’t focus, felt hopeless. She nearly quit. Then she tracked her symptoms and realized: the fatigue started the day she began the pill. The hopelessness? It had been there for months. The pill wasn’t making her worse-it was just causing tiredness while slowly helping her mood.
Another man thought his arthritis was flaring. He was in pain every morning. Turns out, his blood pressure med was causing muscle cramps that felt like joint pain. Switching drugs fixed it.
These aren’t rare. A 2022 survey of over 12,000 patients found 63% had mistaken a side effect for their disease. The most common mix-ups? Sleep problems, stomach issues, and brain fog.
What’s Changing in Medicine
Hospitals are starting to use AI tools that look at your health records and flag possible side effects. One system, MedAware’s SafetyRx, predicts side effects with 91% accuracy by comparing your symptoms to millions of other patient records.
Genetic testing is becoming more common too. Some labs can tell if you’re more likely to have side effects from certain drugs based on your DNA. Insurance now covers this for high-risk meds like warfarin or certain antidepressants.
And wearables? Apple’s Heart Study showed smartwatches can now tell the difference between a drug-induced irregular heartbeat and one caused by heart disease-with 88% accuracy.
This isn’t science fiction. It’s happening now.
Your Next Steps
Here’s what to do today:
- Look at your meds. When did you start each one?
- Write down any new symptoms and when they began.
- Check if they match known side effects for your drugs (use MedShadow.org or your pharmacy’s website).
- Start a simple journal-just a note in your phone or a sticky note.
- Ask your doctor or pharmacist: ‘Could any of these symptoms be from my meds?’
You don’t need to be a doctor to spot the difference. You just need to pay attention. Your body is talking. Learn its language. And don’t assume every new feeling means your disease is getting worse. Sometimes, it’s just the pill.



Adam Rivera
January 14 2026Man, I wish my doctor had told me this six months ago. I thought my SSRIs were making me depressed-turns out I just needed to wait it out. The fatigue? Side effect. The sadness? Been there since college. Sometimes the body just needs time to adjust, y’know?