Hydrocortisone Usage Calculator
Calculate Safe Usage
Get personalized recommendations based on your acne situation and usage patterns
Usage Recommendation
Acne can be frustrating, especially when over‑the‑counter options don’t clear the skin fast enough. A common question that pops up is whether hydrocortisone - a cream many people keep in their first‑aid drawer for rashes - can actually help an occasional breakout without causing more trouble. Below we explore how it works, who might benefit, and the safety trade‑offs you should weigh before slathering it on your face.
What is Hydrocortisone?
Hydrocortisone is a low‑potency corticosteroid that mimics the body’s own cortisol hormone. It’s categorized as a Topical steroid, meaning it’s applied directly to the skin to calm inflammation, reduce redness, and suppress the immune response that fuels swelling. Over the counter, you’ll usually find 0.5% or 1% strengths in creams, ointments, or lotions.
Why would anyone consider it for acne?
Acne isn’t just a clogged‑pore problem; it’s heavily driven by inflammation. When a pore gets blocked, bacteria such as Propionibacterium acnes multiply, triggering an immune response that leads to the painful, red bumps we associate with the condition. Because hydrocortisone directly tampers with that inflammatory cascade, it can quickly reduce the size and colour of a blemish.
Dermatologists often reserve it for short‑term use on isolated, inflamed lesions that haven’t responded to standard acne products. It’s not a primary acne therapy, but rather a rapid‑acting rescue for those occasional, stubborn spots.
Which types of acne might benefit?
The cream works best on papules and pustules - the raised, inflamed types that are painful to the touch. It’s less useful for non‑inflammatory comedones (whiteheads and blackheads) or for deep cystic lesions that require systemic treatment. If you have oily skin, frequent breakouts, or hormonal acne, a topical steroid alone won’t address the root causes like excess sebum or hormonal fluctuations.
Safety profile - what are the risks?
Like any medication, hydrocortisone isn’t risk‑free. The most common side effects include skin thinning, dryness, and a temporary lightening of the skin where it’s applied. Overuse can lead to perioral dermatitis - a rash that forms around the mouth and nose - or even trigger steroid addiction, where the skin becomes dependent on the cream to stay calm.
The cream should never be used on large areas of the face, for longer than a week, and definitely not on broken skin or active infections. The FDA classifies low‑strength hydrocortisone as safe for short‑term, limited‑area use, but it also warns that prolonged exposure can increase the risk of systemic absorption, especially on delicate facial skin.
How to apply correctly
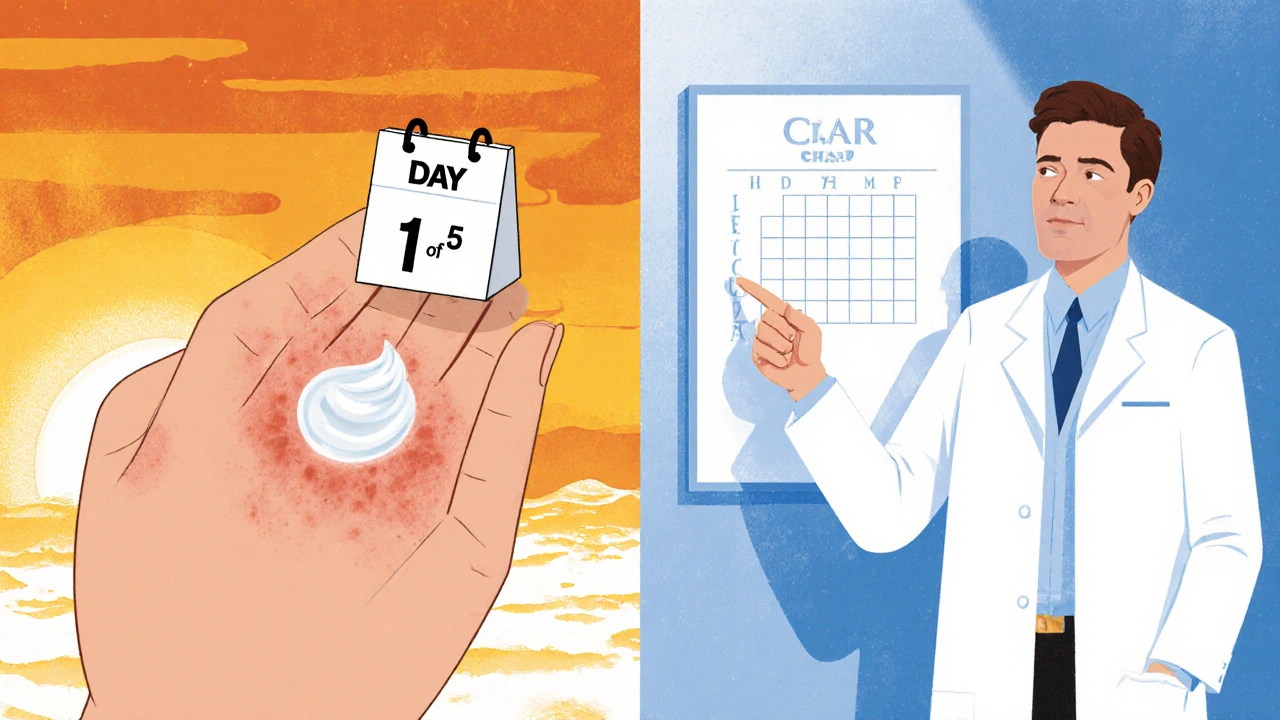
- Wash the affected area with a gentle cleanser and pat dry.
- Apply a pea‑size amount to the inflamed spot only. Gently rub in; avoid the surrounding skin.
- Limit use to once or twice a day for a maximum of 5‑7 days.
- After the course, switch to a non‑steroidal acne treatment (e.g., Benzoyl peroxide or a retinoid) to keep the inflammation under control.
Never combine hydrocortisone with other potent topical actives like high‑strength retinoids or salicylic acid in the same routine - the mix can increase irritation and skin barrier damage.
How does it stack up against other acne treatments?
| Treatment | Mechanism | Typical OTC Strength | Pros | Cons |
|---|---|---|---|---|
| Hydrocortisone | Anti‑inflammatory steroid | 0.5‑1% | Fast reduction of redness; easy to apply | Skin thinning, limited to short‑term use, not effective on non‑inflammatory lesions |
| Benzoyl peroxide | Antibacterial, keratolytic | 2.5‑10% | Kills acne bacteria; reduces pore blockage | Can cause dryness, bleaching of fabrics |
| Salicylic acid | Beta‑hydroxy acid, exfoliator | 0.5‑2% | Clears comedones; gentle for sensitive skin | May irritate if over‑used; slower results on inflamed lesions |
| Retinoids (adapalene) | Modulates cell turnover, anti‑inflammatory | 0.1‑0.3% | Prevents new lesions; smooths texture | Initial irritation; sun sensitivity; prescription for stronger forms |
Real‑world scenarios
Scenario 1 - A single inflamed pimple before a big event: A one‑time, 0.5% hydrocortisone application can calm the swelling within hours, letting you walk into the venue without a visible blemish.
Scenario 2 - Recurrent inflammatory acne on the jawline: Relying on steroids repeatedly will thin the skin and possibly worsen breakouts. Here, a regimen of a topical retinoid combined with a mild benzoyl peroxide wash is more sustainable.
Scenario 3 - Sensitive, eczema‑prone skin that also breaks out: Because hydrocortisone also eases eczema flare‑ups, a dermatologist might prescribe a combined steroid‑antibiotic cream (e.g., clindamycin‑hydrocortisone) to tackle both issues safely.
When to see a professional
If you find you need hydrocortisone more than twice a month, if lesions spread beyond a few spots, or if you notice persistent dryness, cracking, or discoloration, book an appointment with a Dermatologist. They can evaluate whether you need prescription‑strength steroids, oral antibiotics, hormonal therapy, or a different acne protocol altogether.
Key takeaways
- Hydrocortisone is a short‑term fixer for inflamed blemishes, not a long‑term acne solution.
- Limit use to 5‑7 days on a small area to avoid skin thinning and other side effects.
- Combine it with a proven acne routine after the steroid course ends.
- Consult a dermatologist if you need frequent or wide‑area applications.
Can I use hydrocortisone on my entire face?
No. Hydrocortisone should only be applied to isolated, inflamed lesions for a short period. Using it on large facial areas can cause skin thinning and systemic absorption.
How long should I keep using hydrocortisone for a pimple?
Limit the treatment to a maximum of five to seven days. If the spot hasn’t improved after that, stop using the cream and try another acne product.
Will hydrocortisone make my skin more oily?
It doesn’t increase oil production, but the cream can temporarily mask the skin’s natural barrier, leading to a feeling of greasiness. Follow up with a lightweight moisturizer.
Is it safe to combine hydrocortisone with benzoyl peroxide?
Generally avoid using them at the same time. Benzoyl peroxide can degrade the steroid, reducing its efficacy, and the combo may increase irritation.
What should I do if I notice skin thinning after using hydrocortisone?
Stop the steroid immediately. Switch to a gentle, barrier‑repair moisturizer containing ceramides and consider seeing a dermatologist for further guidance.



Tammy Sinz
October 22 2025Hydrocortisone exerts its anti‑inflammatory effect primarily via high‑affinity binding to intracellular glucocorticoid receptors, which subsequently translocate to the nucleus and suppress NF‑κB‑mediated transcription of pro‑inflammatory cytokines such as IL‑1β and TNF‑α. This mechanistic pathway explains the rapid diminution of erythema observed in isolated papular lesions. However, the drug’s pharmacodynamics also involve down‑regulation of fibroblast proliferation, accounting for the well‑documented risk of dermal atrophy with prolonged exposure. Clinicians therefore recommend a “spot‑treat” approach, limiting application to a pea‑sized amount on a single lesion for a maximum of five to seven days. In practice, this protocol balances the acute therapeutic benefit against the cumulative risk of barrier compromise.