Why Metoprolol Isn’t Always the Golden Ticket
Metoprolol has a rep as a bit of a go-to when it comes to managing high blood pressure or protecting the heart. Doctors reach for it because it works for most people—notice, I said most. That’s where things get tricky. Every body is different, and for some, metoprolol can be like wearing shoes that just don’t fit. Maybe you know the feeling: taking your daily dose, only to get hit with low energy, brain fog, or even a pounding headache. I’ve spoken to folks who’ve had to ditch favorite hobbies because the fatigue was just too much. Others landed in the doctor’s office because of slow heartbeats or worsened asthma. Let’s not ignore that occasionally, serious side effects—like severe allergic reactions or dramatic drops in blood pressure—can hit out of nowhere. And if you have particular conditions like asthma, COPD, or certain heart blocks, taking metoprolol can actually do way more harm than good. Not everyone is willing to tough it out for the sake of lower blood pressure, and that’s a reasonable call. Nobody should be stuck with a drug that doesn’t work for them just because it’s popular. The good news: modern medicine has plenty of alternate routes.
Getting Real: When Symptoms Demand a Switch
Let’s talk symptoms. It’s way too easy to brush off weird feelings as “normal” side effects, especially when you’re eager to manage your blood pressure or heart rhythm. But here’s a tip: if you regularly feel dizzy standing up, your heart rate dips below 50 beats per minute, or you’re gasping when going up the stairs, these aren’t just issues to accept. I’m always surprised when folks put up with stuff like erectile dysfunction or extreme fatigue, thinking it’s just part of getting treated. Sure, metoprolol is well-researched for reducing risks after a heart attack and tackling angina, but if your quality of life tanks, you need a better fit. Pay hard attention to new or worsening depression, odd moods, or sleep struggles after starting the drug. Folks with diabetes should also stay extra alert—metoprolol can mask warning signs of low blood sugar. If any of these symptoms get in your way, have a frank chat with your doctor. Bring a list of what you’ve noticed, when it happens, and how it’s holding you back. Be honest—this info is pure gold for finding the right swap. And remember, no one solution works for every heart or every life. What matters is finding what lets you keep living the way you want.
Alternatives That Pack a Punch (and Are Backed by Science)
Swapping out metoprolol doesn’t mean you’re stuck without options. In fact, there are a handful of medication groups that tackle the same heart and blood pressure issues but in different ways—and each comes with its own personality. Beta-blockers like atenolol, bisoprolol, or carvedilol share some traits with metoprolol but sometimes play nicer with certain body types or coexisting conditions. Atenolol, for instance, has a longer-lasting effect in the body, so your schedule might get simpler. Carvedilol has extra benefits for heart failure because it also blocks alpha receptors, helping relax blood vessels even more. For those who just can’t handle beta-blockers, calcium channel blockers (like amlodipine or diltiazem) step in with muscle-relaxing superpowers that ease blood flow without the bradycardia (slow heart rate) issue. If blood pressure is the main enemy, ACE inhibitors (like lisinopril) or angiotensin II receptor blockers (ARBs like losartan) are serious contenders—these have been the mainstays in blood pressure clinics for decades and offer bonus protection for kidneys (especially for people with diabetes). Looking to see all your options neatly in one spot? There’s an excellent breakdown of medication swaps in alternative for metoprolol. That resource lays out risk profiles, how the drugs work, and some useful charts to help you compare. Research in the last few years has truly shifted how we sequence medications, so don’t think you’re stuck with old advice.
What to Expect When Making the Switch
Switching medications isn’t as simple as just stopping one pill and starting another—it should always be done under a doctor’s watchful eye. Sudden stops, especially with beta-blockers like metoprolol, can sometimes cause “rebound” effects. That means your blood pressure or heart rate shoots up, and your risk for chest pain or arrhythmias can increase. Your doctor might lower your dose gradually or overlap with the new med until your body adjusts. Be clear on what a transition plan looks like—ask about how to watch for headache, swelling, or weird heartbeats as your new drug kicks in. Some meds start working within a few days. Others, like certain ACE inhibitors, could take up to two weeks to reach full effect. Try to keep your routine as consistent as possible through the change: eat similar foods, stick to regular exercise, and keep sleep steady. One smart move: monitor your blood pressure and pulse at home. You don’t need a high-tech setup—a basic cuff from the pharmacy works just fine. Tracking your numbers not only reassures you, it gives your doctor a goldmine of info for follow-ups. It’s also totally normal to feel anxious about switching or worry something will go wrong. Don’t keep those worries bottled up—a good doctor wants to hear them. Most patients find finding the right fit is a game changer. You gain your energy back and, often, learn new ways your body responds to medications.
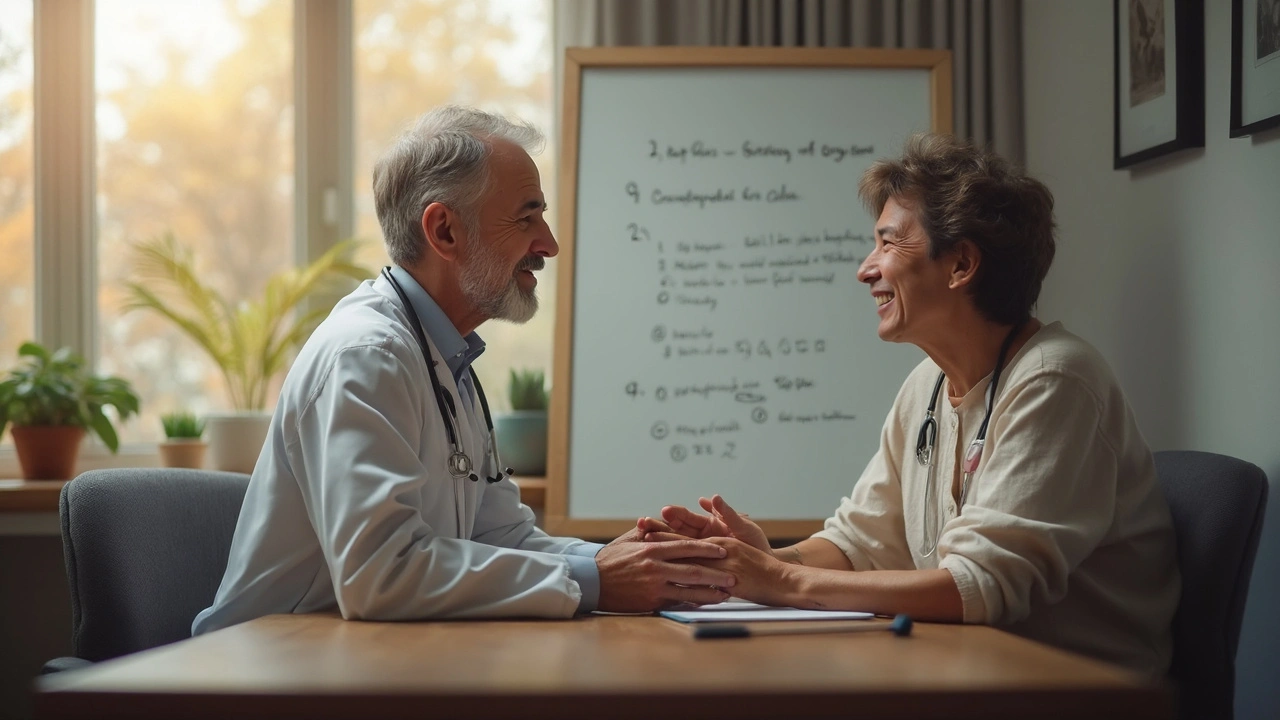
Talking With Your Doc: Tips for Getting What You Need
Doctors may know the science inside out, but you’re the expert on how you feel day to day. Start with specifics. Saying “I feel tired” is OK, but saying “By 2 PM, I can barely keep my eyes open—it never happened before metoprolol” is much more powerful. Bring notes if you have to. Don’t forget to mention your lifestyle, too: sports you love, work demands, or even family responsibilities that require you to be alert and active. If money is an issue, talk about it—many heart medications have cheaper generics, and there are even patient assistance programs out there. Ask what side effects are common with the alternatives, and which need urgent attention. If your doctor starts with another beta-blocker, push for what’s different about it compared to metoprolol. Curious about a certain drug you saw in a commercial or read about in a heart group? Bring that up—it’s your right to understand what’s on offer. For many folks, adding in a low sodium diet, more daily steps, or weight loss can be just as powerful as the medication swap. Make sure your whole health plan, not just your prescription, is on the table during your visit.




Nina Vera
July 17 2025Oh wow, this is such a critical topic! Metoprolol really isn't for everyone, and sometimes it feels like docs just hand it out like candy without considering alternatives thoroughly.
I've had friends who struggled horribly with side effects, and honestly, it can be so scary when your heart meds don’t suit you. I'm super curious about these alternatives you mentioned—are any supposed to be gentler on energy levels? Because that crash feeling from beta blockers can be brutal.
Plus, the idea of having practical tips to discuss med changes with doctors is huge. Sometimes it feels like they don’t hear you, right?
Would love to hear real stories from others too, cause nothing beats lived experience when it comes to meds and managing side effects.