Every year, nearly half a million people in the U.S. get Lyme disease - but only about 30,000 are officially counted. Why? Because many cases go undiagnosed, misdiagnosed, or slip through the cracks of a system that still struggles to recognize the early signs. If you’ve ever had unexplained fatigue, joint pain, or a strange rash after a hike or yard work, you’re not alone. And the clock starts ticking the moment a tick bites you.
How Lyme Disease Starts - And How Fast
Lyme disease isn’t caused by just any tick. It’s spread by blacklegged ticks - specifically Ixodes scapularis in the East and Ixodes pacificus on the West Coast. These ticks are tiny. Nymphs, the most dangerous stage, are no bigger than a poppy seed. You might not even feel them.The bacteria behind Lyme, Borrelia burgdorferi, doesn’t jump into your blood right away. It takes time. Most sources agree: if the tick is removed within 24 hours, your risk drops by 95%. But research shows transmission can begin as early as 15 hours, especially if the tick is already engorged. That’s why checking yourself after being outdoors isn’t optional - it’s critical.
The CDC recommends showering within two hours of coming inside and doing a full-body tick check. Look in the armpits, behind the knees, in the hairline, and around the waist. Ticks don’t burrow - they latch on and feed. The longer they stay, the higher the chance they pass on the bacteria.
The Three Stages of Lyme Disease - And What Happens in Each
Lyme disease doesn’t happen all at once. It unfolds in stages, and each one has its own symptoms - and its own window for treatment.Stage 1: Early Localized (1-28 days after bite)
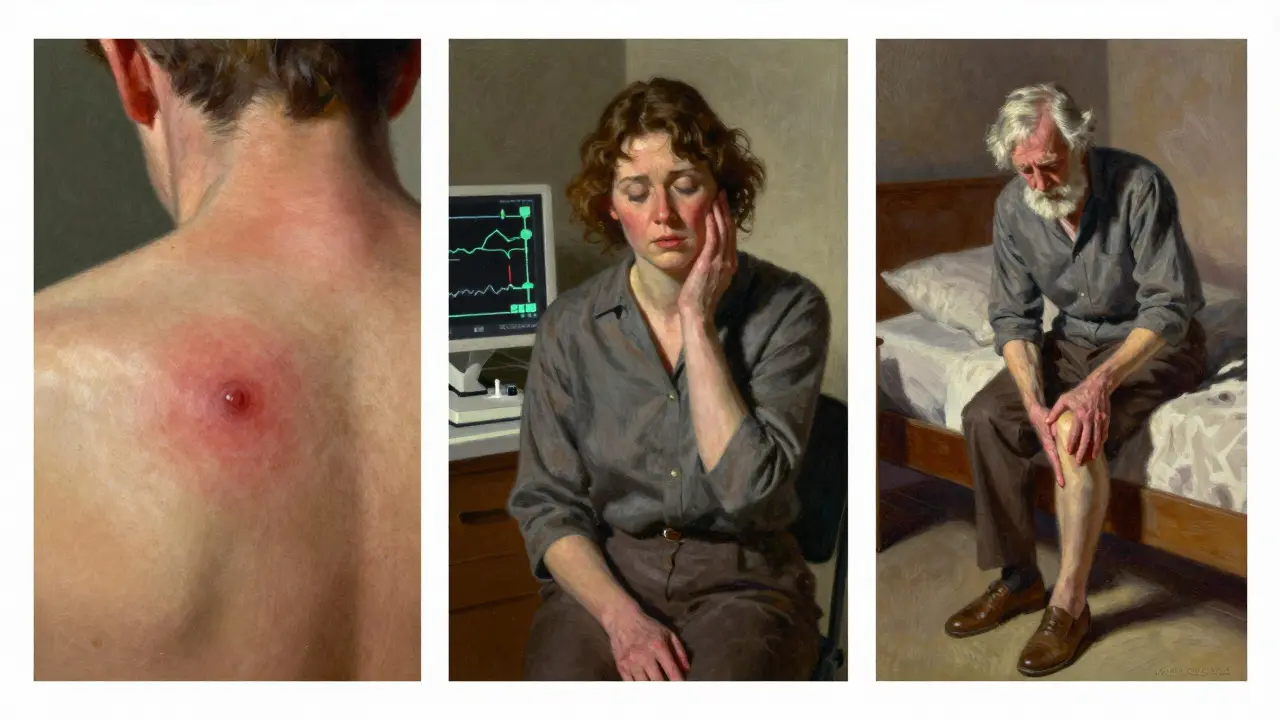
This is your best chance to stop Lyme before it spreads. About 70-80% of people develop a rash called erythema migrans - the classic "bull’s-eye" rash. It starts as a small red spot and expands over days, sometimes clearing in the center. But not everyone gets it. Some people only feel flu-like symptoms: fever (45%), headaches (61%), fatigue (70%), chills, or muscle aches.
If you see this rash, you don’t need a blood test. The rash alone is a diagnosis. Dr. Allen Steere, who first identified Lyme disease, said it’s pathognomonic - meaning it’s unique to Lyme. Start treatment immediately.
Stage 2: Early Disseminated (weeks to months after bite)
If Stage 1 is missed, the bacteria spread. Now you’re in Stage 2. Symptoms become more serious and scattered. You might get multiple rashes. Nerve damage can cause facial palsy - one side of your face droops, like Bell’s palsy. Heart problems can show up too: Lyme carditis, which causes irregular heartbeat, dizziness, or fainting. About 4-10% of untreated cases develop this.
Joint pain starts here too, but it’s usually mild. Still, this is the stage where misdiagnosis is common. People are told they have the flu, arthritis, or even a neurological disorder. Blood tests at this point are more reliable - but not perfect. They can still miss 35% of early cases because your body hasn’t made enough antibodies yet.
Stage 3: Late Disseminated (months to years after bite)
This is what happens when Lyme goes untreated for too long. About 60% of people develop severe arthritis - often in the knees. Pain comes and goes. Nerve damage can lead to numbness, tingling, or burning sensations. Cognitive issues like brain fog, memory loss, and trouble focusing are common. Some patients describe it as "mental slowness" - like their thoughts are stuck in mud.
At this stage, damage can be long-lasting. That’s why early treatment matters so much.
Treatment Timeline - What Works, When, and Why
Antibiotics are the only proven treatment. There’s no magic cure, no herbal remedy that replaces them. But timing and type matter.
Stage 1: Oral Antibiotics
For early Lyme, doctors prescribe 10-21 days of oral antibiotics. Adults get doxycycline. Kids and pregnant women get amoxicillin or cefuroxime. Doxycycline kills the bacteria fast and also prevents other tick-borne illnesses like anaplasmosis. It’s not just a Lyme drug - it’s a broad-spectrum shield.
Studies show 87% of patients treated within 30 days of symptoms recover fully within three months. That’s the gold standard.
Stage 2 and 3: IV Antibiotics
If the infection reached the nervous system or heart, you need stronger treatment. That means intravenous antibiotics like ceftriaxone or penicillin G for 14-28 days. This isn’t optional. Delaying IV treatment increases the risk of permanent nerve or joint damage.
Some patients worry about IV antibiotics being "overkill." But if your doctor recommends it, it’s because your case has crossed a line. Don’t wait. Don’t hope it gets better. This isn’t a mild cold.
Prophylaxis - One Dose Can Prevent It All
If you find an engorged blacklegged tick attached for more than 36 hours in a high-risk area (Northeast, Mid-Atlantic, Upper Midwest), you may be eligible for a single 200mg dose of doxycycline within 72 hours of removal. This cuts infection risk by 87%. It’s not for everyone - only when all the conditions line up - but if you’re in the right place at the right time, it’s a game-changer.
The Controversy - Chronic Lyme, PTLDS, and What Experts Really Say
Here’s where things get messy. Some patients feel tired, achy, or foggy for months after finishing antibiotics. That’s not "chronic Lyme." That’s Post-Treatment Lyme Disease Syndrome (PTLDS).
PTLDS affects 10-20% of treated patients. It’s not an active infection. It’s your body still healing - inflammation, nerve sensitivity, or lingering immune response. Studies show antibiotics don’t help PTLDS. In fact, long-term antibiotics can cause serious harm: C. diff infections, liver damage, antibiotic resistance.
The Infectious Diseases Society of America (IDSA) says this clearly: no evidence supports prolonged antibiotics for PTLDS. But the International Lyme and Associated Diseases Society (ILADS) disagrees. They argue some patients need longer courses. And 28 U.S. states have passed laws protecting doctors who prescribe them.
The truth? There’s no consensus. But science says: don’t take antibiotics for months. Do focus on rest, physical therapy, and managing symptoms. Many patients with PTLDS improve over 6-12 months with supportive care.

What’s New in 2025 - Diagnostics, Vaccines, and Hope
There’s progress. In March 2023, the FDA approved the first new Lyme diagnostic test in 20 years: MiQLick. It detects bacterial DNA in urine - not antibodies. That means it can catch Lyme earlier, even before your immune system responds. Sensitivity? 92%. Specificity? 95%.
Vaccines are coming too. Valneva’s VLA15 vaccine, backed by Pfizer, showed 70-96% effectiveness in Phase 2 trials. It targets multiple strains of Borrelia. Human trials are underway, and if approved, it could be available by 2027.
Researchers at NIAID are also testing an mRNA Lyme vaccine - the same tech used in COVID shots. Early animal results are promising. Human trials start in mid-2024.
And climate change? It’s making things worse. Ticks are moving north. In Canada, their range expanded 50% between 2000 and 2020. By 2050, Lyme cases could double. Prevention isn’t just smart - it’s urgent.
What You Should Do Right Now
- If you find a tick - remove it with tweezers. Grasp close to the skin. Pull straight up. Don’t twist, burn, or smother it with oil.
- Save the tick in a sealed bag. Note the date and location. If you get sick, it helps doctors.
- If you see a bull’s-eye rash - start antibiotics immediately. Don’t wait for a test.
- If you’re in a high-risk area and had an engorged tick for over 36 hours - ask your doctor about the single-dose doxycycline.
- If you’re still tired or achy after treatment - see a specialist. PTLDS is real. But it’s not Lyme. Treat the symptoms, not the ghost.
Lyme disease isn’t a death sentence. It’s not a mystery. It’s a time-sensitive infection - and the clock starts the moment a tick bites. Know the signs. Act fast. Don’t wait for a lab report when your body is screaming for help.
Can you get Lyme disease from a dog or cat?
No. Dogs and cats can get Lyme disease from ticks, but they can’t pass it to humans. The only way you get Lyme is through the bite of an infected tick. However, if your pet brings ticks into your home, you’re at higher risk of being bitten. Use tick preventatives on pets and check them after outdoor time.
Do all ticks carry Lyme disease?
No. Only blacklegged ticks (Ixodes species) carry the bacteria that cause Lyme disease. Even among those, not every tick is infected. In high-risk areas, 20-50% of nymphs may carry the bacteria. In low-risk areas, it’s under 5%. The key isn’t avoiding all ticks - it’s knowing which ones are dangerous and how to remove them quickly.
Can you get Lyme disease more than once?
Yes. Getting Lyme once doesn’t make you immune. You can be reinfected if bitten again by another infected tick. That’s why prevention - tick checks, repellents, protective clothing - is lifelong, even after you’ve had it before.
Are blood tests for Lyme disease reliable?
They’re helpful - but flawed. In the first few weeks, blood tests miss up to 35% of cases because your body hasn’t made antibodies yet. By Stage 2, accuracy improves to 87%. The two-step test (ELISA + Western blot) is standard, but false positives happen too. Never rely on a test alone. If you have symptoms and a known tick bite, treat clinically - don’t wait for results.
What should you do if antibiotics don’t seem to work?
First, make sure you took the full course. Then, rule out other causes - like other tick-borne illnesses (anaplasmosis, babesiosis) or autoimmune conditions. If symptoms persist after treatment, you may have PTLDS. Talk to a Lyme specialist. Focus on symptom management: physical therapy, sleep hygiene, stress reduction, and pacing. Don’t start long-term antibiotics without strong evidence - the risks outweigh the benefits.
Is Lyme disease only a problem in the Northeast?
No. While 95% of cases are reported in 14 northeastern and midwestern states, ticks are spreading. Cases are now confirmed in nearly every state. Southern ticks carry different bacteria, but blacklegged ticks are moving into new areas due to warmer temperatures and deer populations. If you spend time outdoors anywhere in the U.S., you’re at some level of risk.



lisa Bajram
January 9 2026Okay but can we talk about how wild it is that we’re still using 20-year-old diagnostics in 2025? 😅 I got bit last summer in Vermont, went to three docs, got two negative tests, and still had that bullseye rash - they wanted to wait for bloodwork. I started doxy on my own after reading this. Saved my summer. 🙌