When someone is trying to quit drinking, the right medication can make all the difference. But here’s the part no one talks about enough: medications for alcohol use disorder don’t work in a vacuum. Take them without the right support, ignore side effects, or accidentally mix them with alcohol - and you could be setting yourself up for a relapse, even if you’ve been sober for months.
How These Medications Actually Work
There are three FDA-approved pills for alcohol use disorder, each with a different job. They’re not magic bullets. They’re tools. And like any tool, they only help if used correctly.Acamprosate (brand name Campral) helps calm the brain after you’ve stopped drinking. It doesn’t stop cravings. It doesn’t make you sick if you drink. What it does is fix the chemical imbalance caused by long-term alcohol use. Think of it like patching up a leaky pipe after you’ve turned off the water. It’s most effective for people who’ve already detoxed and want to stay completely sober. You have to take it three times a day - six pills total. That’s a lot to remember. And if you miss doses, it loses its power.
Naltrexone (Revia, Vivitrol) works differently. It blocks the part of your brain that makes alcohol feel rewarding. If you drink while on naltrexone, the high fades. It doesn’t make you sick - it just takes the joy out of it. That’s why it’s often better for people who aren’t ready for total abstinence yet. They still drink, but they drink less. The extended-release shot, Vivitrol, is given once a month. No daily pills. But you can’t start it until you’ve been off opioids for at least a week. And if you’re using it to cut back, not quit, you still need to be careful. One study showed it didn’t stop people from drinking at all - just reduced the number of heavy drinking days.
Disulfiram (Antabuse) is the oldest of the three. It’s also the most extreme. If you drink while taking it, your body can’t break down alcohol properly. You get a brutal reaction: pounding headache, vomiting, sweating, chest pain, even low blood pressure. It’s designed to scare you off alcohol. But here’s the catch: it only works if you take it. And if you forget - or worse, if you drink anyway - the reaction can be dangerous. Many people quit because of the side effects: metallic taste, drowsiness, or just the fear of accidentally drinking something with alcohol, like mouthwash or cough syrup.
Why People Stop Taking Their Medication
The science says these drugs work. But real life? It’s messier.In clinical trials, about 60% of people stayed on acamprosate or naltrexone for 16 weeks. That sounds okay - until you realize the placebo group had the same rate. The real problem comes after that. Real-world data shows only about one in three people are still taking their medication after three months.
Why? Cost is a big one. Even though most are generic, acamprosate can run $200-$300 a month. Naltrexone, especially the shot, costs up to $400. That’s a lot if you’re paying out of pocket. Disulfiram? Only $20-$50. But even that’s too much for some.
Side effects matter too. One in ten people on acamprosate get diarrhea. Naltrexone can cause nausea. Disulfiram? Almost everyone complains about the taste. And then there’s the emotional toll. People feel like they’re being controlled by a pill. One person on a recovery forum said, “I took naltrexone for two months. I didn’t get drunk, but I didn’t feel like myself either. So I stopped.”
And then there’s the timing. You can’t start acamprosate until you’ve been sober for three to five days. If you’re still drinking, you have to wait. That’s a long time to stay off alcohol without any help. Naltrexone needs a seven-day gap if you’ve used opioids. That’s another barrier.

The Hidden Relapse Triggers
Relapse doesn’t happen because someone “just wanted a drink.” It happens because something broke.One common mistake? Thinking the medication will fix everything. You take naltrexone, but you don’t go to therapy. You don’t change your environment. You still hang out with people who drink. You still keep beer in the fridge. The pill reduces cravings, but it doesn’t erase habits. Without behavioral support, the risk of relapse stays high.
Another? Mixing medications. The COMBINE study tested whether combining acamprosate and naltrexone worked better. It didn’t. One pill was just as good as two. But some doctors still prescribe both, especially if the patient is struggling. That increases side effects and cost - without adding benefit.
And then there’s liver health. Naltrexone is processed by the liver. If you have cirrhosis or even mild liver damage from years of drinking, your doctor needs to monitor your enzymes every month. If they don’t, you could be putting extra stress on a damaged organ. Gabapentin, which isn’t FDA-approved for AUD but is often used off-label, is safer here. It’s cleared by the kidneys, not the liver. For someone with alcohol-related liver disease, gabapentin might be the smarter choice.
Disulfiram? Don’t even think about it if your liver is already damaged. It can cause severe liver toxicity. Yet, some patients still get prescribed it - often because it’s cheap and easy to write a prescription for.
Who Gets the Best Results?
Not everyone responds the same way. That’s the key point doctors are starting to understand.If you’ve had severe withdrawal symptoms - seizures, hallucinations, delirium tremens - gabapentin might be your best bet. One 2020 study found 45% of people with heavy withdrawal history stayed sober on gabapentin, compared to just 28% on placebo. If you’ve never had bad withdrawal, it barely helped at all.
If you’re trying to quit cold turkey and stay completely sober, acamprosate is your friend. It helps you feel normal again. If you’re trying to cut back - maybe have one drink on weekends without losing control - naltrexone gives you more flexibility.
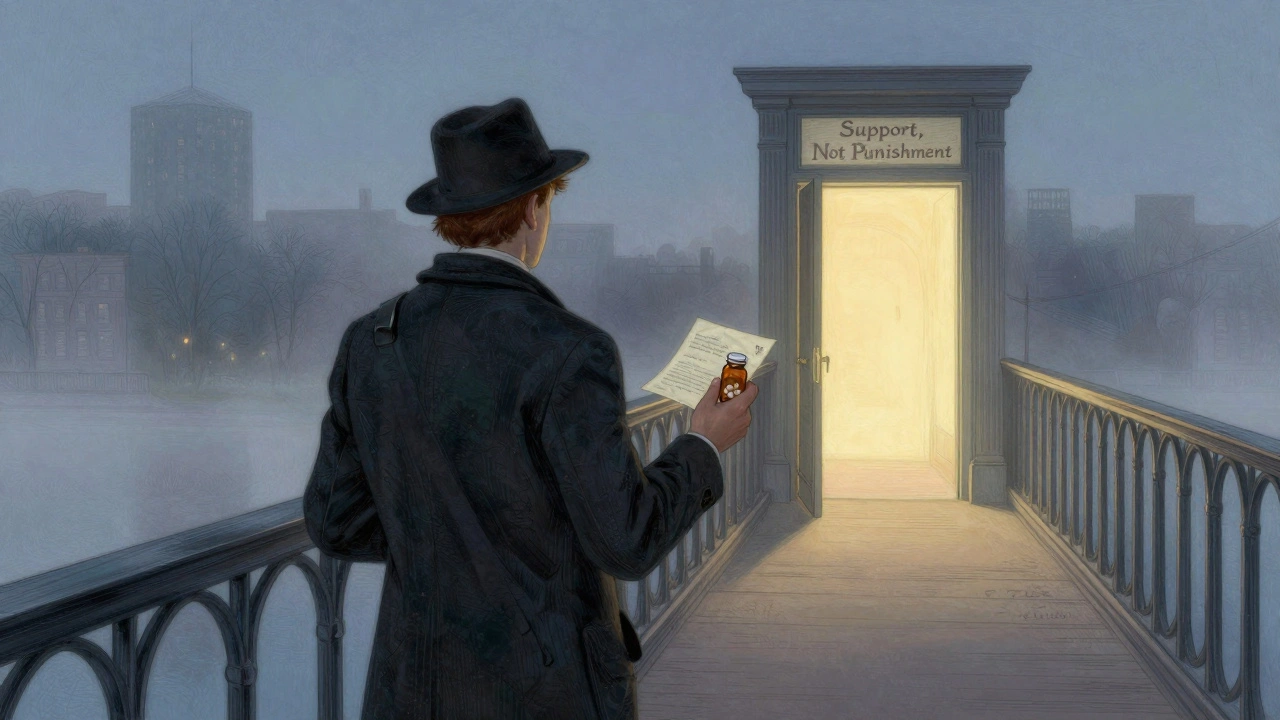
And disulfiram? It only works if you’re terrified of drinking. If you’re motivated by fear, it can be powerful. But if you’re motivated by hope, by rebuilding your life - it’s the wrong tool. It’s punishment, not support.
What’s Changing in Treatment Right Now
The field is moving fast. New tools are emerging.There’s a new version of acamprosate that’s just two pills a day instead of six. That alone could improve adherence. There’s also a 6-month naltrexone implant in early trials. If it works, it could solve the biggest problem: remembering to take your pill.
Then there’s digital help. Apps that track cravings, send reminders, and connect you to counselors. One 2023 study found combining these with medication cut relapse risk by 33%. That’s huge.
And science is getting smarter. Researchers are now using brain scans to predict who will respond to acamprosate. People with certain patterns in their frontal white matter had a 68% better chance of staying sober on the drug. That’s not science fiction - it’s happening now.
Even the microbiome is being studied. Some early trials show that specific probiotics and supplements can reduce heavy drinking days by nearly 40%. It’s early, but it’s promising.
What You Should Do
If you’re on medication for alcohol use disorder:- Don’t skip doses - even one missed day can weaken the effect.
- Don’t drink alcohol, even a sip. The consequences aren’t worth it.
- Get regular blood tests if you’re on naltrexone or disulfiram - liver and kidney health matter.
- Pair medication with counseling, support groups, or an app. The pill doesn’t work alone.
- Talk to your doctor about your goals. Are you trying to quit completely? Cut back? That changes which medication is right for you.
- If you can’t afford your meds, ask about patient assistance programs. Many drug companies offer them.
If you’re thinking about starting medication:
- Be honest with your doctor about your drinking history - especially if you’ve had withdrawal.
- Ask: “Which of these drugs fits my lifestyle?” Not “Which one is best?”
- Don’t be afraid to switch. If one doesn’t work, another might.
- Know the side effects before you start. Don’t wait until you’re sick to ask questions.
Medications for alcohol use disorder are powerful. But they’re not a cure. They’re a bridge. And if you don’t cross the bridge carefully - if you ignore the risks, skip the support, or forget the rules - you might end up right back where you started.
Can I drink alcohol while taking naltrexone?
Technically, yes - naltrexone doesn’t make you sick if you drink. But it’s not safe or smart. The whole point of naltrexone is to reduce the reward from alcohol. Drinking while on it defeats the purpose. It also increases your risk of relapse because you’re not learning new behaviors. Plus, heavy drinking while on naltrexone can still damage your liver. Don’t do it.
Why is acamprosate only for people who are already sober?
Acamprosate works by restoring balance in your brain after alcohol withdrawal. If you’re still drinking, your brain chemistry is still being disrupted. The medication can’t do its job. You need at least 3-5 days of complete abstinence before starting. Trying to take it while drinking is like trying to fix a leak while the faucet is still on.
Is disulfiram worth the risk?
Only for a very specific type of person: someone who is highly motivated, understands the reaction, and has a strong support system. It’s not for people who might accidentally drink - like those who use alcohol-based mouthwash or eat food cooked with wine. The side effects are real, and the risk of severe reactions is high. Most doctors avoid it unless other options have failed.
Can I take gabapentin instead of naltrexone or acamprosate?
Gabapentin isn’t FDA-approved for alcohol use disorder, but it’s commonly used off-label - especially for people with a history of withdrawal or liver problems. Studies show it helps reduce cravings and prevents relapse in those with severe withdrawal symptoms. It’s safer for the liver than naltrexone and doesn’t require abstinence before starting. Talk to your doctor if you’ve had bad withdrawal or liver damage.
How long should I stay on AUD medication?
There’s no one-size-fits-all answer. Most studies look at 6-12 months. But alcohol use disorder is a chronic condition, like high blood pressure or diabetes. Many people benefit from staying on medication longer - even years. If you’re doing well and have support, there’s no reason to stop just because a trial ended. Talk to your doctor about long-term use. Stopping too soon is one of the biggest reasons people relapse.
What if I can’t afford my medication?
Cost is a major barrier, but help exists. Most AUD medications have generic versions. Acamprosate and disulfiram are often under $50 a month with coupons. Naltrexone is more expensive, but many pharmaceutical companies offer patient assistance programs. Call the manufacturer - they often provide free or discounted meds to people who qualify. Also, check with local health departments or addiction treatment centers. Many offer free or low-cost medication programs.



Emmanuel Peter
December 5 2025Let me tell you something no one wants to admit - these meds are just corporate bandaids. The real problem? You’re not broken, you’re traumatized. But hey, why fix the system when you can sell a pill that makes people feel like they’re doing something? I’ve seen guys on naltrexone still showing up to AA meetings drunk as hell, just quieter. The system profits from dependency, not recovery.