Every year, millions of Americans take generic drugs. They’re cheaper, widely available, and approved by the FDA. But when something goes wrong-when a generic version of levothyroxine doesn’t seem to work like the brand, or when a patient breaks out in a rash after switching to a new batch of sertraline-how does the FDA find out? The answer lies in MedWatch, the U.S. Food and Drug Administration’s voluntary safety reporting system. For generic medications, this system is both essential and deeply flawed.
What MedWatch Actually Does
MedWatch isn’t a fancy lab or a government database with secret algorithms. It’s a simple reporting portal where doctors, pharmacists, nurses, and even patients can submit details about bad reactions, drug failures, or product defects. Since 1993, it’s been the backbone of post-market drug safety in the U.S. When someone reports a problem with a generic pill-say, dizziness after switching from one manufacturer to another-that report goes into the FDA Adverse Event Reporting System (FAERS). FAERS holds over 9 million reports as of 2023. Most of them involve drugs. And nearly half of those involve generics.Why Generics Are Hard to Track
Here’s the problem: when you report a bad reaction to “generic sertraline,” the system doesn’t know if it came from Teva, Mylan, or a little-known manufacturer in India. The form asks for the drug name, the event, and your contact info. That’s it. No manufacturer. No lot number. No National Drug Code (NDC). And that’s a huge gap. In 2024, FDA data showed that only 32.7% of reports mentioning generics included the manufacturer’s name. Compare that to brand-name drugs, where 89.4% of reports correctly named the maker. That means the FDA is flying blind on most generic safety signals. Two patients might have the same reaction to “generic bupropion,” but if one report says Mylan and the other says Sandoz, the system can’t connect the dots. That’s why experts call this the “generic identification problem.”Therapeutic Inequivalence: The Silent Issue
Patients don’t always report “side effects.” Sometimes they report “it just doesn’t work anymore.” That’s therapeutic inequivalence-the feeling that the generic version isn’t doing what the brand did. It’s not always about chemistry. It’s about inactive ingredients. Fillers. Coatings. Even the shape of the pill can change how fast a drug gets absorbed. A 2022 study found that patients switching from brand to generic levothyroxine often report fatigue, weight gain, or brain fog. These aren’t rare. They’re common enough that the FDA added “therapeutic failure” as a specific reporting category in MedWatch. One pharmacist in Ohio submitted 17 MedWatch reports over three years about generic levothyroxine. Only two got replies. But one led to a label change. That’s the power of persistence. But most patients don’t know how to report. Or they don’t know which manufacturer made their pills. A 2023 FDA survey found 63% of consumers couldn’t name the maker of their generic medication.
Who Reports-and Why It Matters
Healthcare professionals are the most reliable reporters. A 2024 AMA survey showed 96% of physicians found MedWatch easy to use. But only 28.3% of consumer reports included the NDC code-the unique identifier printed on the pill bottle. That’s the key. If you report “generic metformin,” and you don’t include the NDC, the FDA can’t trace it back to the factory. Pharmacists know this. They’re trained to check the NDC. But they’re also overworked. In a 2024 ASHP survey, 71% of pharmacists said they didn’t have time to fill out detailed reports. Patients? They’re the most numerous reporters, but the least informed. Many think “generic” means “same as brand.” When they feel worse, they blame their condition, not the pill. The FDA’s own data shows that only 4.7% of all drug-related adverse event reports mention “generic” as a factor. That’s not because generics are safe. It’s because the problem isn’t being reported.How the FDA Is Trying to Fix It
The FDA knows this is a problem. In 2024, they rolled out a new algorithm to automatically spot generic drugs in FAERS reports. It uses patterns in drug names, manufacturer codes, and timing of reports. It’s 92.4% accurate at identifying generics. That’s a big leap. But it’s still a workaround. It doesn’t fix the root issue: people aren’t giving enough detail. The Generic Drug User Fee Amendments (GDUFA) III plan, launched in 2023, promised to improve this. One goal: make it easier to link reports to specific manufacturers. The next step? Integration with electronic health records by 2026. Imagine this: you’re prescribed a generic. Your doctor’s system automatically logs the NDC. When you report a reaction, the system pulls the manufacturer, lot number, and dose. No guesswork. No missing info.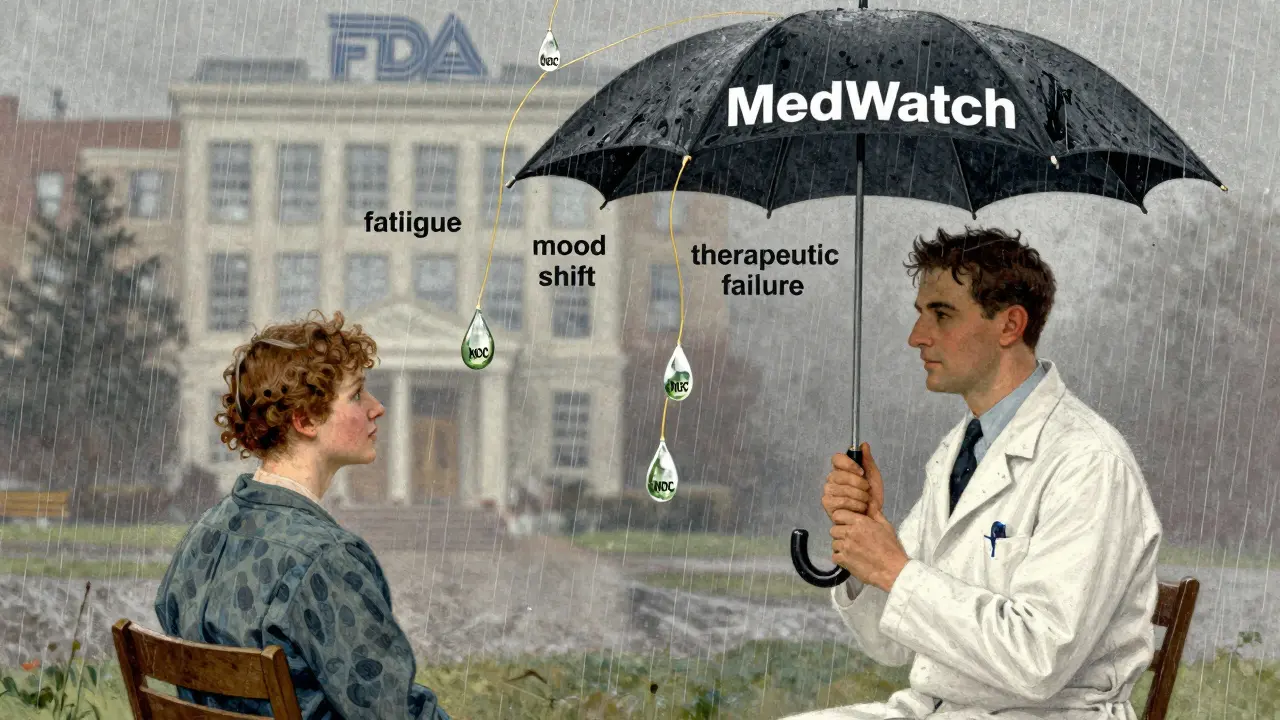
What You Can Do
If you’re a patient: check your pill bottle. Look for the NDC number. It’s a 10-digit code, usually near the barcode. Write it down. If you notice a change in how you feel after switching generics-fatigue, nausea, mood swings, or lack of effect-don’t assume it’s your body. Report it. Go to www.fda.gov/MedWatch. Fill out the form. Even if you don’t know the manufacturer, write “unknown.” Better to report something incomplete than nothing at all. If you’re a clinician: always record the NDC when prescribing or dispensing generics. If a patient says, “This generic doesn’t work like the last one,” don’t dismiss it. Ask: which one? Who made it? That’s the data the FDA needs. Submit a report. It takes 15 minutes. You might be the one who triggers a label change-or even a recall.The Bigger Picture
Generics make up 90% of prescriptions in the U.S. But they account for only 23% of drug spending. That’s why manufacturers compete on price, not on packaging details. But safety isn’t cheap. When a generic version of bupropion XL caused seizures in multiple patients in 2022, it was MedWatch reports that started the investigation. Within 11 months, the FDA updated the label. That’s how the system should work. Right now, it’s broken. Too many reports are vague. Too many manufacturers go untracked. Too many patients suffer in silence. But change is coming. The algorithm is better. The tools are improving. The FDA is listening. But it still needs you.MedWatch isn’t magic. It’s a tool. And tools only work if people use them correctly. For generics, that means reporting with details. Naming the maker. Writing the NDC. Not assuming “generic” means “identical.” Because sometimes, it’s not.
Can I report a bad reaction to a generic drug even if I don’t know the manufacturer?
Yes. The FDA accepts reports even without the manufacturer name. But the more detail you provide-like the National Drug Code (NDC) from the pill bottle, the date you started the medication, and how your symptoms changed-the more useful your report becomes. If you don’t know the manufacturer, write “unknown.” Better to report with partial info than not at all.
Why do some people say generic drugs don’t work as well as brand-name ones?
Generics must meet FDA bioequivalence standards-they must deliver 80-125% of the active ingredient compared to the brand. But inactive ingredients like fillers, dyes, or coatings can affect how quickly the drug is absorbed. Some patients are sensitive to these changes. Reports of fatigue, mood shifts, or reduced effectiveness after switching generics are common, especially with drugs like levothyroxine, sertraline, and warfarin. These aren’t always “side effects”-they’re signs of therapeutic inequivalence.
How does the FDA tell which generic manufacturer caused a problem?
Right now, they mostly rely on the NDC code, which is unique to each manufacturer and product. But only 28% of consumer reports include it. The FDA uses a new algorithm to guess the manufacturer based on drug name patterns and timing, but it’s not perfect. If multiple reports point to the same NDC or manufacturer name, the FDA can flag a potential issue. That’s how they identified problems with Mylan’s bupropion XL in 2022.
Are generic drugs less safe than brand-name drugs?
No. The FDA requires generics to meet the same quality, strength, and purity standards as brand-name drugs. Most generics are safe and effective. But because there are dozens of manufacturers for a single generic drug, small differences in manufacturing can lead to variations in how patients respond. These aren’t safety failures-they’re performance variations. That’s why tracking reports by manufacturer matters.
How long does it take for the FDA to act on a MedWatch report?
There’s no fixed timeline. Most reports are reviewed for patterns, not individually. If 10 or more similar reports come in about the same generic drug and manufacturer, the FDA may investigate. That can take weeks or months. In rare cases-like the bupropion XL issue in 2022-it took 11 months from the first report to a label change. It’s slow, but it works when enough people report.
Can I report a problem if I got my generic drug from outside the U.S.?
Yes. The FDA accepts reports for any medication used in the U.S., even if it was imported. Include as much detail as possible: the drug name, manufacturer (if known), where you bought it, and the NDC if available. The FDA tracks imported drugs too, especially as more generics come from overseas facilities.




Paige Shipe
December 29 2025The FDA’s MedWatch system is a joke. Millions of people take generics every day, and the agency can’t even track which company made the pill? That’s not oversight-it’s negligence. I’ve had three different batches of levothyroxine and each one made me feel like a zombie. I reported it twice. No reply. No follow-up. Just silence. The system isn’t broken-it was designed this way to protect Big Pharma’s bottom line.