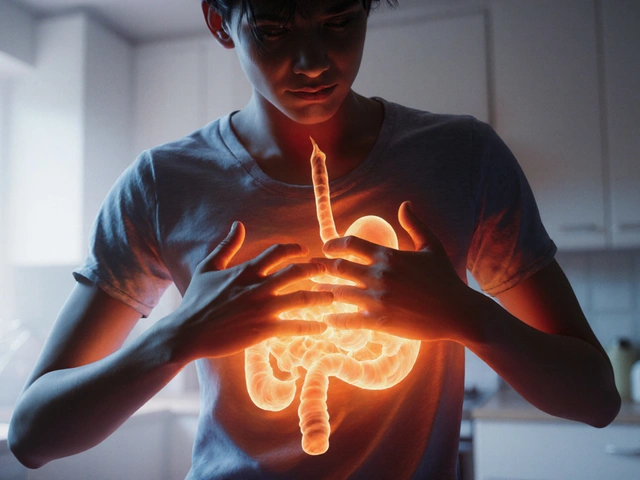
Stomach ulcer is a chronic sore in the stomach lining, often caused by excess acid, Helicobacter pylori infection, or prolonged NSAID use. When the protective mucus thins, even ordinary meals can provoke burning pain, nausea, or bleeding.
Why Your Diet Matters
Food isn’t just fuel; it directly contacts the ulcer‑prone lining. Certain ingredients increase gastric acid, irritate nerves, or slow healing. Adjusting what you eat can cut flare‑ups by up to 40% according to a 2022 gastroenterology review.
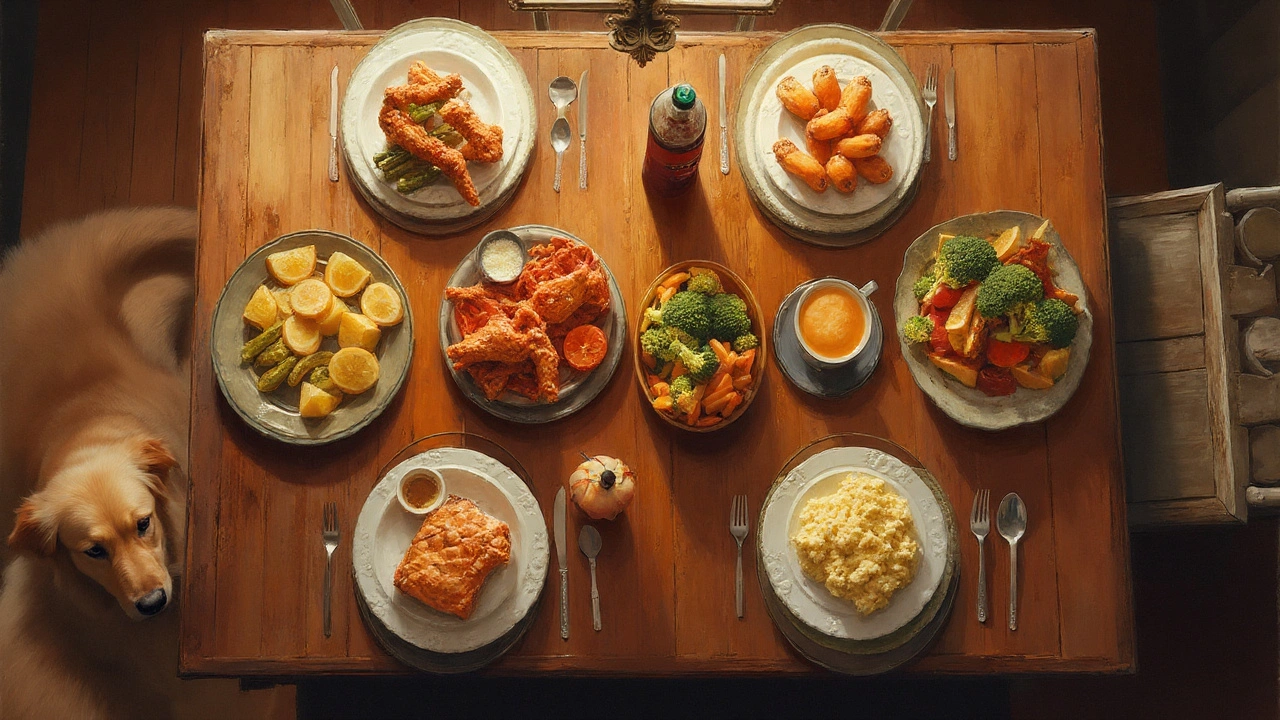
The Top 10 Trigger Foods
Below is the definitive list of foods to avoid for stomach ulcers. Each entry shows what it is, why it hurts, and a common serving size that often sneaks into meals.
- Spicy foods are dishes that contain chili peppers, hot sauce, or strong spices. The capsaicin in pepper can stimulate acid secretion and heighten pain sensitivity.
- Acidic foods include tomatoes, vinegar‑based dressings, and pickles. Their low pH adds extra acid load, overwhelming the already thin mucus barrier.
- Caffeinated beverages such as coffee, black tea, and energy drinks raise gastrin levels, prompting the stomach to pump more acid.
- Alcoholic beverages irritate the mucosa and impair blood flow, slowing ulcer healing and making the lining more vulnerable.
- Carbonated drinks (soda, sparkling water) introduce bubbles that expand in the stomach, increasing pressure and reflux of acid.
- Fried foods are high‑fat items like chips, fried chicken, and onion rings. Fat delays stomach emptying, allowing acid to linger longer.
- Citrus fruits (oranges, grapefruits, lemons) carry natural citric acid that can aggravate an ulcer‑scarred lining.
- Chocolate contains caffeine and theobromine, both of which stimulate acid production; it’s also rich in fat.
- Peppermint relaxes the lower esophageal sphincter, promoting reflux that can carry acid up to the ulcer site.
- Processed meats (sausages, salami) are high in salt and preservatives that increase stomach irritation.
How These Foods Worsen an Ulcer
Each trigger attacks the ulcer in a slightly different way:
- Acid‑boosting: caffeine, coffee, chocolate, and alcoholic drinks raise gastrin, a hormone that tells the stomach to secrete more hydrochloric acid.
- Direct irritation: hot sauces, pepper, and citrus physically scrape the already thin mucus.
- Delayed emptying: fatty or fried foods keep food in the stomach for longer, letting acid act for extended periods.
- Mechanical pressure: carbonated drinks expand, forcing acid upward and creating reflux.
Smart Substitutes That Soothe
Swapping one trigger for a gentler option can make a huge difference. Here are practical replacements:
- Replace spicy sauces with mild herb‑based dressings (basil, parsley, lemon‑zest oil).
- Choose low‑acid vegetables like cucumber, zucchini, and leafy greens instead of tomatoes.
- Swap coffee for decaf tea or warm water with a slice of ginger.
- Opt for non‑alcoholic mocktails made with herbal teas and fresh fruit juice (diluted, no citrus).
- Drink still water or herbal infusions rather than soda.
- Grill or bake lean proteins (chicken breast, fish) instead of deep‑frying.
- Enjoy ripe bananas or melons as a sweet snack - they’re low‑acid and gentle on the stomach.
Quick Comparison of the Top Triggers
| Food | Acidity (pH) | Spice/Fat Level | Typical Serving | Reason to Avoid |
|---|---|---|---|---|
| Spicy sauces | ~5.5 | High | 1 tbsp | Capsaicin spikes acid |
| Tomatoes | ~4.3 | Moderate | ½ cup diced | Low pH adds extra acid |
| Coffee | ~5.0 | Low | 8oz | Caffeine raises gastrin |
| Red wine | ~3.5 | Low | 5oz | Alcohol irritates mucosa |
| Soda | ~2.5 | Low | 12oz | Carbonation ↑ pressure |
| Fried chicken | ~6.0 | High | 1 piece (≈120g) | Fat delays emptying |
| Citrus juice | ~2.8 | Low | ½ cup | Citric acid irritates lining |
| Chocolate bar | ~5.8 | Medium | 1oz | Caffeine + fat load |
Related Concepts You Might Encounter
Understanding ulcer care goes beyond food avoidance. These topics often appear alongside dietary advice:
- Helicobacter pylori - a bacteria that can cause or worsen ulcers; testing and eradication therapy are common.
- Proton pump inhibitors (PPIs) - medications that reduce acid production, allowing the ulcer to heal.
- Stress management - chronic stress can increase acid secretion, so relaxation techniques help.
- Fiber‑rich diets - soluble fiber (oats, applesauce) may protect the lining and support healing.
- Smoking cessation - tobacco reduces mucus production and impairs blood flow.
When to Seek Medical Help
If you notice any of these signs, book an appointment promptly:
- Severe, persistent gnawing pain lasting more than a few hours. \n
- Dark, tar‑like stools or bright red blood in vomit.
- Unexplained weight loss or loss of appetite.
- Symptoms that don’t improve despite dietary changes.
Early diagnosis and a tailored treatment plan-including diet, medication, and lifestyle tweaks-give the best chance for a swift recovery.
Frequently Asked Questions
Can I ever eat spicy food again after an ulcer heals?
Yes, most doctors recommend re‑introducing spicy dishes gradually once the ulcer has fully closed-usually after 4‑6 weeks of treatment. Start with mild peppers and monitor any discomfort.
Is caffeine always bad for ulcer patients?
Caffeine itself raises gastrin, but a small cup of decaf coffee is usually tolerated. The key is to keep total caffeine under 100mg per day and avoid strong espresso.
Do carbonated drinks delay ulcer healing?
The bubbles increase intra‑gastric pressure, which can force acid back onto the ulcer site. Switching to still water or herbal tea reduces that mechanical stress.
Are there any foods that actively help ulcer recovery?
Foods rich in flavonoids (e.g., blueberries, apples, kale) and those high in mucilage (e.g., oatmeal, bananas) coat the stomach lining and may speed healing.
How long should I stay away from alcohol after diagnosis?
Most gastroenterologists advise complete abstinence for at least 4‑6 weeks while the ulcer heals, then a moderate limit (no more than one standard drink per day) if you wish to re‑introduce it.



Samantha Dean
September 21 2025It is commendable that the article delineates the physiological mechanisms by which certain foods exacerbate gastric ulceration, thereby providing a rational framework for dietary modification. The emphasis on acid‑stimulating agents such as caffeine and capsaicin aligns with current gastroenterological consensus, and the inclusion of specific serving sizes offers practical guidance. Moreover, the discussion of non‑acidic alternatives reflects an integrative approach to patient care.