When a doctor prescribes a generic version of a brand-name drug, most patients don’t think twice. But for many, there’s an invisible barrier - not about cost, not about effectiveness, but about story. The brand-name drug comes with a history: a slick commercial, a familiar logo, a doctor’s confident tone. The generic? A plain pill in a white bottle. No story. No emotional weight. And that makes all the difference.
Why Generic Drugs Feel Like Second Best
People don’t just take pills. They take meaning. A brand-name medication like Lipitor or Prozac isn’t just chemistry - it’s a promise. It’s tied to years of advertising, TV jingles, and doctor recommendations. It feels like progress. Like science. Like safety. Generic drugs? They’re chemically identical. The FDA requires them to work the same way. But without a story, they feel like placeholders. Patients worry: "Is this really the same?" "Did they cut corners?" "Will it even work for me?" This isn’t irrational. It’s human. Our brains are wired to trust narratives more than data. A 2022 study in the Journal of Consumer Psychology found that patients who heard a personal story about someone successfully using a generic drug were 47% more likely to accept it than those who only received a fact sheet on bioequivalence.Narrative Medicine: The Missing Link
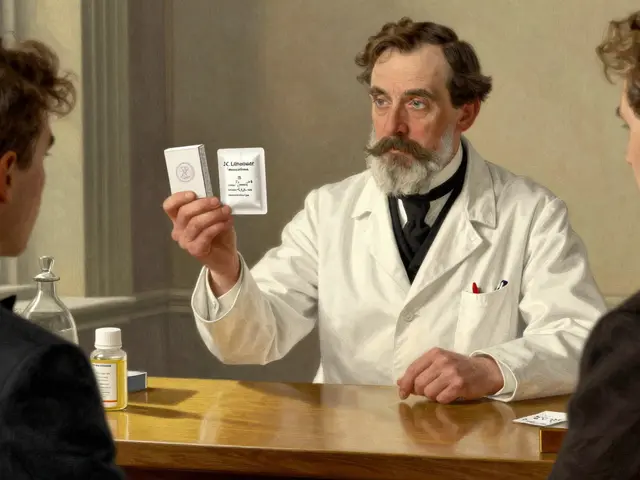
Enter narrative medicine - not as a soft add-on, but as a clinical tool. Developed by Dr. Rita Charon at Columbia University in the late 1990s, narrative medicine teaches clinicians to listen not just to symptoms, but to the stories behind them. It’s about paying attention to what’s said - and what’s left unsaid. In practice, this means asking: "What does this medication mean to you?" or "Have you had a bad experience with a generic before?" One nurse in a rural clinic in Kentucky started using this approach after noticing her elderly patients refusing generic blood pressure pills. Instead of explaining bioavailability, she asked: "Tell me about the last time you took a pill that didn’t feel right." One patient, a retired teacher, replied: "My husband took the blue pill for ten years. He lived. Then they switched him to the white one. He got dizzy. Died three months later. I don’t trust the white ones." The nurse didn’t correct him. She listened. Then she said: "That’s a heavy story. Let me show you something." She pulled up the FDA’s database showing that the generic version he was now being given was made by the same company that produced the original blue pill - just under a different label. She showed him the exact same active ingredient, the same manufacturing standards. Then she asked: "Would it help if we called it by the same name your husband knew?" He agreed. The next prescription was labeled with the original brand name in parentheses: "Lisinopril (Prinivil) - generic." He took it. His blood pressure stabilized. And he started telling others: "It’s the same pill. Just a different bottle."
How Stories Rewire Belief
The brain doesn’t process facts the same way it processes stories. When you hear a statistic - "98% bioequivalence" - your prefrontal cortex evaluates it. When you hear a story - "My neighbor took this pill and walked her dog again" - your limbic system lights up. Emotion becomes memory. Memory becomes belief. Narrative medicine doesn’t try to convince patients they’re wrong. It meets them where they are. It takes their fear, their grief, their confusion - and gives it shape. Then it gently adds new details. A 2023 study in The Permanente Journal followed 300 patients prescribed generic antidepressants. Half received standard counseling. The other half received a 15-minute narrative session: "Tell me about your journey with medication. What did you hope it would do? What scared you?" After six weeks, 72% of the narrative group reported full adherence. Only 41% of the control group did. Why? Because the narrative group didn’t just understand the science - they felt seen. Their fear wasn’t dismissed. It was honored. And then, gently, recontextualized.How Clinicians Can Start Using Narrative Medicine Today
You don’t need a degree in literature to use narrative medicine. You just need to slow down. Here’s how:- Ask open-ended questions: "What do you know about this medication?" not "Do you know what this is?"
- Listen for metaphors: If a patient says, "I don’t want to be on this pill forever," they’re not talking about chemistry - they’re talking about identity.
- Use their words: If they call the generic "the cheap one," don’t correct them. Say: "Tell me more about what ‘cheap’ means to you."
- Share a story - carefully: "I had a patient last month who felt the same way. Then she learned the truth. Would you like to hear what happened?"
- Write it down: Keep a notebook. Not of diagnoses - of stories. Over time, you’ll see patterns. You’ll learn which fears are common. Which myths need to be gently untangled.

Why This Matters Beyond Pills
This isn’t just about generic drugs. It’s about how we communicate trust in healthcare. A patient who accepts a generic medication is more likely to stick with their treatment plan. They’re more likely to refill prescriptions. Less likely to end up in the ER. Less likely to feel ashamed for "cheating" their way to care. Narrative medicine doesn’t replace science. It makes science human. In a world where patients are bombarded with ads, misinformation, and rushed appointments, a story - real, quiet, honest - becomes the most powerful medicine of all.The Bigger Picture
The rise of narrative medicine isn’t a trend. It’s a correction. For decades, medicine celebrated objectivity. Numbers. Lab results. Algorithms. But the human experience of illness doesn’t live in a spreadsheet. It lives in silence, in hesitation, in tears, in the way someone says, "I just can’t take another pill." Narrative medicine asks: What if we treated stories like vital signs? What if we measured not just blood pressure - but belief? What if we recognized that the most effective drug isn’t the one with the strongest molecule - but the one with the strongest story behind it? Generic drugs aren’t inferior. They’re misunderstood. And stories - real, patient-centered stories - are the bridge. The future of healthcare isn’t just about better science. It’s about better listening. And that starts with one question: "Tell me what this means to you."Is narrative medicine just about listening, or is there actual training involved?
Narrative medicine isn’t just passive listening - it’s a skill set that requires training. Programs like the one at Columbia University teach clinicians how to read literature, analyze metaphors in patient speech, and reflect on their own emotional responses to stories. Clinicians learn to identify what’s missing in a patient’s narrative - the silence between words, the body language, the repeated phrases - and use those clues to guide care. It’s not therapy. It’s clinical attention refined through humanities training.
Can narrative medicine really change whether someone takes a generic drug?
Yes. Research shows that when patients hear a relatable story about someone else successfully using a generic medication - especially when it addresses their specific fears - their willingness to accept it increases significantly. In one study, patients who participated in a 15-minute narrative session were nearly twice as likely to adhere to their generic prescription compared to those who only received standard counseling. The story doesn’t change the drug - it changes the meaning attached to it.
Does narrative medicine work with all types of patients?
It works best when adapted to the individual. Some patients want to tell long stories; others prefer short, direct answers. Some are skeptical at first. The key isn’t forcing storytelling - it’s creating space for it. Even a single question like, "What are you most worried about with this medication?" can open the door. Narrative medicine meets people where they are, whether they’re quiet, angry, confused, or hopeful.
How is narrative medicine different from patient education?
Patient education tells. Narrative medicine listens. Patient education says, "Here’s why the generic works." Narrative medicine says, "Tell me why you think it doesn’t." It doesn’t assume the patient needs fixing - it assumes they need understanding. One gives facts. The other gives meaning. Both matter, but only narrative medicine addresses the emotional resistance that often blocks adherence.
Are there any risks to using storytelling in healthcare?
The biggest risk is when clinicians use stories to manipulate or oversimplify. Telling a patient, "My cousin took this and it worked great!" can backfire if it feels dismissive. Effective narrative medicine doesn’t replace evidence - it deepens it. The goal isn’t to convince patients they’re wrong. It’s to help them feel heard so they can reconsider their beliefs on their own terms. Done well, it builds trust. Done poorly, it erodes it.



Chelsea Harton
January 17 2026stories are the only thing that makes medicine feel real.
facts don't save lives. people do. and people remember stories.
why do you think ads work?
it's not the science. it's the feeling.
we're all just animals with better grammar.