Stevens-Johnson Syndrome (SJS) and Toxic Epidermal Necrolysis (TEN) aren’t just rare skin conditions-they’re medical emergencies that can turn a routine medication into a life-threatening event. These conditions start with what feels like the flu, then rapidly spiral into skin and mucous membrane destruction. If you’ve ever taken an antiseizure drug, an antibiotic like sulfamethoxazole, or even a common painkiller like ibuprofen, you should understand how dangerous these reactions can be-even if they’re rare.
What’s the Difference Between SJS and TEN?
For decades, doctors treated SJS and TEN as two separate diseases. Now we know they’re part of the same deadly spectrum. The only real difference is how much of your skin comes off.
SJS affects less than 10% of your body surface area. TEN? That’s more than 30%. There’s even a middle zone-10% to 30%-called SJS/TEN overlap. The more skin that detaches, the higher your risk of dying. In SJS, about 5% to 15% of people don’t survive. In TEN, that number jumps to around 25%.
Think of it like a severe burn, but it’s not caused by heat. It’s your own immune system turning on your skin and mucous membranes. The blisters don’t form from friction or infection-they just peel away on their own.
How Does It Start?
It usually begins with a fever over 102°F, sore throat, cough, burning eyes, or just feeling really sick for no clear reason. This phase lasts a day or two. Then, without warning, red or purple spots appear on your chest or back. They look like targets or bruises, not typical rashes.
Within 24 to 72 hours, those spots turn into blisters. The skin starts to slough off in large sheets. If you rub the area, the top layer peels away easily-that’s called the Nikolsky sign, and it’s a major red flag.
But here’s what most people don’t realize: your mouth, eyes, and genitals are often hit just as hard-if not harder-than your skin. Around 90% of patients have painful mouth sores that make eating or drinking impossible. Eight out of ten have eye damage. Six in ten develop genital sores. These aren’t minor annoyances. They can lead to permanent blindness, urinary blockages, or scarring that lasts a lifetime.
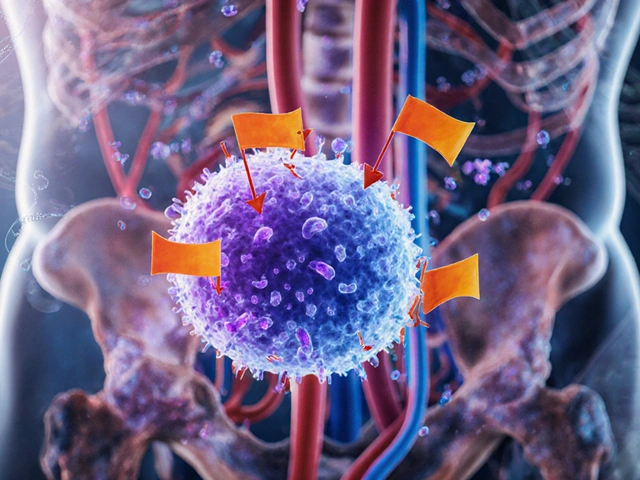
What Causes It?
Over 80% of cases are triggered by medications. The usual suspects:
- Antiseizure drugs: Carbamazepine, phenytoin, lamotrigine (account for about 30% of cases)
- Sulfa antibiotics: Trimethoprim-sulfamethoxazole (Bactrim, Septra) (about 20%)
- Allopurinol: Used for gout (about 15%)
- NSAIDs: Ibuprofen, naproxen, diclofenac
- Nevirapine: An HIV medication
It’s not just about the drug itself-it’s about your genes. Some people carry a genetic marker called HLA-B*15:02. If you have it and take carbamazepine, your risk of SJS/TEN goes up by 1,000 times. Another marker, HLA-B*58:01, makes allopurinol 80 to 580 times more dangerous.
That’s why in places like Taiwan, doctors now test patients for these genes before prescribing these drugs. Since 2007, SJS/TEN cases from carbamazepine dropped by 80%. The U.S. FDA now recommends testing for high-risk groups, especially people of Asian descent.
Less than 10% of cases come from infections-most commonly Mycoplasma pneumoniae, especially in kids.

How Is It Diagnosed?
There’s no single blood test. Diagnosis relies on three things: your symptoms, your medication history, and a skin biopsy.
A dermatologist takes a small sample of the affected skin. Under the microscope, they look for full-thickness death of the top skin layer-no inflammation, no pus, just dead cells peeling away. That’s the hallmark of SJS/TEN. Other conditions like staph scalded skin syndrome or pemphigus look similar but have different patterns under the scope.
Doctors also use a scoring system called SCORTEN to predict survival chances. It looks at seven things: age over 40, cancer history, heart rate over 120, skin detachment over 10%, high blood sugar, high urea, and low bicarbonate. Each factor adds risk. Three factors? 35% chance of death. Five or more? Nearly 90%.
What Happens in the Hospital?
If you’re suspected of having SJS/TEN, you’re admitted immediately-usually to a burn unit or ICU. Time is everything. The longer you wait, the worse it gets.
First step: stop every non-essential drug. Doctors go through your entire medication list, even supplements, and pull the trigger on anything that could be the culprit. They’ll often use a tool called the Naranjo scale to guess which drug caused it.
Then comes fluid replacement. Your skin is leaking fluid like a third-degree burn. You might need three to four times your normal daily fluid intake just to stay alive.
Wound care is delicate. You’re not treated like a burn patient with ointments and gauze. Instead, non-stick dressings, sterile saline sprays, and gentle cleaning are used. Pain control is critical-many patients need IV opioids.
Ophthalmology teams visit daily. Without aggressive eye care, 50% to 80% of survivors develop chronic dry eyes, corneal scarring, or even blindness. Lubricants, amniotic membrane grafts, and eyelid surgery may be needed.
Treatment: What Works and What Doesn’t
There’s no magic bullet. Many treatments have been tried-and most have failed.
IVIG (intravenous immunoglobulin): Used to be the go-to. It’s expensive and given in huge doses (2-3 grams per kilogram). But large studies show it doesn’t improve survival. It’s still used sometimes, but not because it’s proven.
Corticosteroids: Controversial. They can suppress your immune system, but they also raise your risk of deadly infections. Some doctors use short, high-dose pulses early on-but there’s no consensus.
Cyclosporine: This is one of the few treatments with solid data. A 2016 trial showed patients on cyclosporine had a mortality rate of 12.5% compared to 33.3% in those who didn’t get it. It blocks the immune cells that kill skin cells.
Etanercept: A newer option. It blocks a protein called TNF-alpha that drives inflammation. In a 2019 study of 12 TEN patients treated within 48 hours, none died. In comparison, historical controls had a 31.3% death rate. This is promising-but still being studied.
There’s no standard protocol. Treatment depends on the hospital, the doctor’s experience, and how early you get in.

What Happens After You Survive?
Surviving doesn’t mean you’re done. Sixty to eighty percent of survivors face long-term problems.
- Eye issues: Dry eyes (35%), corneal damage (25%), vision loss (5%)
- Skin changes: Dark or light patches (70%), scarring (40%), nail loss or deformity (25%)
- Genital scarring: Urethral strictures (15%), vaginal adhesions (10%)-often needing surgery
- Psychological trauma: 40% develop PTSD from the hospital experience
Many survivors need lifelong eye drops, skin moisturizers, or physical therapy. Some can’t return to work. Others avoid hospitals entirely because of the trauma.
One woman I read about had to use a catheter for three years after her TEN reaction. Another developed severe dry eye and couldn’t wear contact lenses again. These aren’t rare stories-they’re the norm.
Can It Be Prevented?
Yes-and it’s getting easier.
Genetic testing before starting high-risk drugs is now standard in many countries. If you’re of Asian descent and your doctor wants to prescribe carbamazepine, ask for the HLA-B*15:02 test. If you’re getting allopurinol for gout, ask about HLA-B*58:01. The test is quick, cheap, and can save your life.
Also, never ignore early symptoms. If you start feeling unwell after beginning a new medication-fever, sore throat, rash-stop the drug and get checked immediately. Don’t wait for blisters. Don’t assume it’s just a virus.
Pharmacists and doctors are getting better at flagging risky combinations. But you’re your own best advocate. Know your meds. Know your risks.
What’s Next in Research?
Scientists are working on better ways to predict who’s at risk. The iSCAR consortium is tracking over 1,200 cases worldwide to find new genetic markers.
One breakthrough? A point-of-care test for HLA-B*58:01 that gives results in four hours-not two weeks. The FDA approved it in 2022. That means doctors can test you before giving you allopurinol, and decide right then whether it’s safe.
And then there’s granulysin-a protein released by immune cells that literally kills skin cells. Blocking it could be the next big treatment. Phase II trials for granulysin inhibitors are expected to start in 2024.
But until then, the best defense is awareness: know the signs, know your meds, and act fast.
Can Stevens-Johnson Syndrome be caused by infections?
Yes, but it’s rare. About 10% of cases, especially in children, are triggered by infections like Mycoplasma pneumoniae. Most cases-over 80%-are caused by medications. If you develop a rash and fever after being sick, it’s still important to get checked, but drug reactions are far more common.
Is Stevens-Johnson Syndrome contagious?
No, it’s not contagious. You can’t catch it from someone else. It’s an immune reaction to a drug or infection in your own body. Being near someone with SJS/TEN poses no risk to you.
How long does it take to recover from SJS/TEN?
The acute phase lasts 8 to 12 days, but full recovery can take months. Skin regrows, but scarring and pigmentation changes may remain. Eye and genital complications often require ongoing care. Many survivors deal with chronic dry eyes, pain, or psychological trauma for years.
Can I take the same drug again if I had SJS/TEN before?
Never. If you’ve had SJS or TEN from a specific drug, you must avoid it-and often similar drugs-forever. Re-exposure can trigger an even faster, more severe reaction. Always inform all your healthcare providers about your history.
Are there any over-the-counter drugs that can cause SJS/TEN?
Yes. Non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen, naproxen, and diclofenac have been linked to SJS/TEN, though less commonly than prescription drugs. Even something as simple as a painkiller you buy at the pharmacy can trigger it in rare cases.
What should I do if I think I’m having a reaction?
Stop taking any new medication immediately. Go to the nearest emergency room. Don’t wait for blisters to appear. Early symptoms like fever, sore throat, and a spreading rash after starting a drug are warning signs. Tell the doctor you suspect Stevens-Johnson Syndrome or Toxic Epidermal Necrolysis. Time is critical.


Dematteo Lasonya
December 4 2025I had a friend go through this after taking ibuprofen for a headache. One day she was fine, the next she was in the ICU. Never thought a painkiller could do that.