NSAID Kidney Risk Calculator
How This Calculator Works
Based on clinical guidelines, this tool estimates your risk of acute kidney injury (AKI) from NSAID use. It's based on factors like age, kidney function, medications, and hydration status.
Your risk level based on current factors
NSAID use may be safe with standard precautions
Consider alternatives and monitor closely
NSAIDs not recommended - consult your doctor
Every year, tens of thousands of people end up in the hospital with sudden kidney damage-not from a virus, not from an accident, but from something they bought off the shelf: ibuprofen, naproxen, or aspirin. These are NSAIDs, the go-to painkillers for headaches, back pain, arthritis, and menstrual cramps. For many, they’re as routine as coffee in the morning. But if you have kidney disease-or even just a few risk factors-you could be walking into a silent danger zone without knowing it.
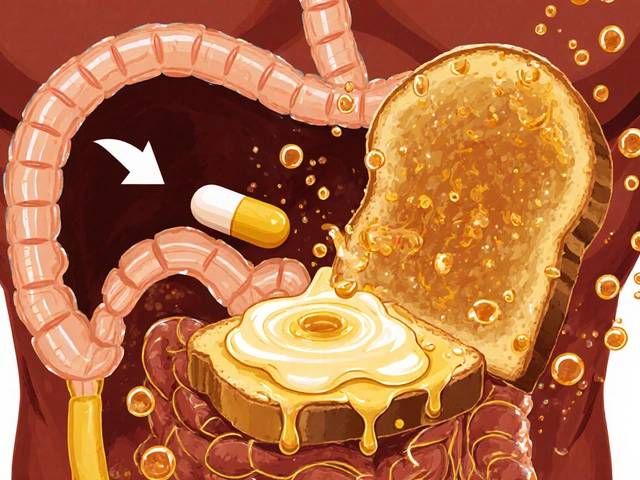
How NSAIDs Hurt the Kidneys
NSAIDs work by blocking enzymes called COX-1 and COX-2, which help make prostaglandins. These tiny molecules aren’t just about inflammation-they’re critical for keeping blood flowing to your kidneys. When you take an NSAID, you cut off that signal. Your kidneys respond by narrowing their blood vessels. That’s fine if you’re healthy and well-hydrated. But if you’re older, dehydrated, or already have kidney trouble, your kidneys can’t compensate. Blood flow drops. Glomerular filtration rate (GFR) can plunge 20-40% within 24 hours. That’s not a slow decline-it’s a sudden drop that can trigger acute kidney injury (AKI).
There are two main ways NSAIDs damage the kidneys. The first, and most common (70-80% of cases), is hemodynamic injury: reduced blood flow leads to ischemia. The second is acute interstitial nephritis (AIN), a rarer immune reaction that causes swelling in the kidney tissue. AIN often comes with fever, rash, or blood in the urine, but many people don’t notice anything until their creatinine levels spike.
Who’s at Risk?
You don’t need to have advanced kidney disease to be vulnerable. Even mild kidney changes raise your risk. Here are the key groups:
- People with eGFR below 60 mL/min/1.73m² (early-stage kidney disease)
- Those over 65 years old
- Patients taking diuretics, ACE inhibitors, or ARBs (especially together-this is the "triple whammy")
- Anyone with heart failure, liver cirrhosis, or volume depletion
- People using NSAIDs daily for months or years
One study found that people with eGFR between 30 and 60 had a 5.8-fold higher risk of AKI after taking NSAIDs. That’s not a small increase-it’s a red flag. And here’s the scary part: up to 30% of early kidney injury cases show no rise in creatinine at all. Your kidneys can be failing, and your blood test looks normal.
The Triple Whammy: When NSAIDs Meet Other Drugs
Combining NSAIDs with ACE inhibitors or ARBs (like lisinopril or losartan) and a diuretic (like furosemide) is like lighting a fuse. Each drug reduces blood flow to the kidneys in a different way. Together, they remove every safety net. A 2013 Medsafe analysis showed this combo increases AKI risk by 31%. But within the first 30 days? Risk jumps to 82% higher. Many patients aren’t warned about this. A 72-year-old man with osteoarthritis and high blood pressure might be taking ibuprofen for pain, lisinopril for BP, and hydrochlorothiazide for fluid retention. He feels fine. Then, after a week, he feels tired. His urine output drops. He’s hospitalized with AKI. All three drugs were prescribed legally. None were flagged as dangerous together.

NSAIDs vs. Alternatives: What’s Safer?
Acetaminophen (Tylenol) is the go-to alternative for pain without inflammation. It carries 40-50% less risk of AKI than NSAIDs. But it doesn’t reduce swelling. If you have arthritis, that’s a problem. Opioids? They don’t hurt the kidneys directly, but they come with addiction risks-15-25% of long-term users develop dependence. Topical NSAIDs (gels, patches) are a smarter choice for joint pain. They deliver the drug straight to the sore spot with 70-80% less absorption into your bloodstream. A 2024 JAMA trial showed 40-50% lower AKI rates with topical NSAIDs compared to pills.
For chronic pain, non-drug options matter: physical therapy, weight loss, heat/cold therapy, and even cognitive behavioral therapy can reduce reliance on pills. In one study, patients with knee osteoarthritis who did 12 weeks of exercise reduced their NSAID use by 60%.
Real Stories, Real Consequences
On Reddit’s r/kidneybros, over 140 people shared stories of NSAID-induced AKI. Most said their doctors never warned them. One man took naproxen for back pain for three weeks. His creatinine went from 1.1 to 7.4. He needed dialysis. Another woman, 68, used ibuprofen daily for 10 years. Her eGFR dropped from 55 to 28 in six months. She didn’t feel sick. Her kidneys just gave out.
These aren’t rare. The National Kidney Foundation estimates 80,000 emergency room visits in the U.S. each year are due to NSAID complications. That’s more than opioid overdoses in some years. And it’s preventable.
How to Protect Your Kidneys
The American Society of Nephrology and KDIGO give clear, practical steps:
- Test first. Before starting long-term NSAID use, get your eGFR and urine albumin-to-creatinine ratio checked. If your eGFR is below 60, talk to your doctor before taking any NSAID.
- Avoid the triple whammy. Never combine NSAIDs with ACE inhibitors, ARBs, and diuretics. If you’re on two of these, NSAIDs are off the table.
- Limit duration. Use NSAIDs for no more than 7-10 days for acute pain. If pain persists, reevaluate. Don’t just keep taking them.
- Monitor weekly. If you must use NSAIDs long-term (e.g., for severe arthritis), check kidney function every week for the first month, then monthly.
- Stay hydrated. Drink 5-10 mL per kg of body weight two to four hours before exercise. During long activity, aim for 0.4-0.8 liters per hour. This keeps urine specific gravity below 1.020 and cuts NSAID-related kidney risk by 60%.
The American Geriatrics Society’s 2023 Beers Criteria says it plainly: NSAIDs should be avoided entirely if your eGFR is below 30. For eGFR 30-60, use only the lowest dose for no more than three days a week.
What You Should Ask Your Doctor
Don’t wait for them to bring it up. Ask these questions:
- "What’s my eGFR? Is it safe for me to take NSAIDs?"
- "Am I on any meds that could interact with NSAIDs?"
- "Are there non-pill options for my pain?"
- "If I start taking this, how will I know if my kidneys are affected?"
If your doctor dismisses your concerns because "it’s over-the-counter," get a second opinion. The FDA hasn’t updated NSAID warnings since 2005. The European Union requires stronger labels. The U.S. hasn’t caught up.
The Future: Better Tools, Safer Pain Relief
Science is catching up. In 2023, the American Society of Nephrology launched the NSAID-RF Risk Calculator. It uses 12 factors-age, blood pressure, eGFR, diuretic use-to predict your 30-day AKI risk with 87% accuracy. It’s not in every clinic yet, but it’s coming.
Researchers are also testing new combinations. One pill combines ibuprofen with acetylcysteine, an antioxidant that may protect kidney tissue. Phase 2 trials are underway. Another breakthrough? Genetic testing. A 2025 Nature study found people with certain PTGS2 gene variants are far more likely to develop kidney injury from NSAIDs. Soon, we might know who’s at high risk before they even take a pill.
Early detection is key. New biomarkers like urinary NGAL can show kidney damage within hours-long before creatinine rises. That means we can stop the injury before it becomes permanent.
Final Takeaway
NSAIDs aren’t evil. They help millions. But they’re not harmless, especially if you have kidney disease or risk factors. The biggest danger isn’t the drug-it’s the assumption that because it’s available without a prescription, it’s safe for everyone. It’s not. Your kidneys don’t scream before they fail. They whisper. And too often, we’re not listening.
If you’re over 60, have high blood pressure, take diuretics, or know your kidneys aren’t perfect-talk to your doctor before the next bottle runs out. There are safer ways to manage pain. You just need to ask for them.



Paul Barnes
January 19 2026NSAIDs don’t cause kidney injury-they’re just the convenient scapegoat for people who won’t take responsibility for their own hydration, diet, or pre-existing conditions.