Most people think of painkillers as harmless-something you grab off the shelf when your head hurts or your back flares up. But what if taking a few extra pills a day for years could quietly destroy your kidneys? This isn’t scare tactics. It’s analgesic nephropathy, a preventable kidney disease caused by long-term use of common pain medications like ibuprofen, naproxen, and even acetaminophen.
What Exactly Is Analgesic Nephropathy?
Analgesic nephropathy is chronic kidney damage from taking large amounts of painkillers over years. It’s not from one bad dose. It’s from the slow, silent buildup-6, 8, or even 10 pills a day, for 3, 5, or 10 years. The kidneys don’t scream. They don’t hurt at first. You won’t feel it until it’s too late.
This condition mostly affects people over 45, especially women. Why women? Many use these drugs daily for migraines, menstrual pain, or arthritis. They don’t see it as dangerous-it’s OTC, after all. But the damage adds up. The kidneys get less blood flow. Toxins build up. The inner parts of the kidney, called papillae, start dying. That’s called papillary necrosis. Over time, scar tissue replaces healthy tissue. The kidneys can’t filter properly anymore.
Back in the 1970s and 80s, this was common because many painkillers contained phenacetin, a now-banned ingredient linked to severe kidney damage. Today, phenacetin is gone. But the problem hasn’t disappeared. NSAIDs like ibuprofen and naproxen, and even acetaminophen, are still the main culprits. The difference? Now it’s harder to spot because the symptoms sneak up slowly.
How Do You Know If It’s Happening to You?
There’s no sudden warning sign. Most people don’t realize they have it until a routine blood test shows elevated creatinine-or they start feeling tired, swollen, or dizzy from high blood pressure.
Early signs are silent:
- Normal urine tests (no protein, no blood)
- Slightly high blood pressure
- Mild fatigue you just chalk up to aging
- Higher-than-normal creatinine on a lab report
By the time you feel pain in your side or notice blood in your urine, the damage is advanced. That’s when kidney tissue starts breaking off and blocking the urinary tract. Some people need dialysis. Others need a transplant.
Here’s the scary part: a 2022 study of 142 patients found that 68% of them didn’t know anything was wrong until their doctor told them. One Reddit user wrote: “I took 8-10 Excedrin Migraine tablets daily for 7 years before my GFR dropped to 45. My nephrologist said I was lucky it wasn’t worse.”
Which Painkillers Are Most Dangerous?
Not all painkillers are equal when it comes to kidney risk.
NSAIDs (ibuprofen, naproxen, aspirin) are the biggest offenders. They block enzymes that help keep blood flowing to the kidneys. Even at normal doses, they can reduce kidney blood flow by 25-40%. Take too much, and that drops to 50-70%. That’s like turning off the water supply to your kidneys.
Acetaminophen was once considered safe for kidneys. But a 2020 study in Kidney International Reports showed that taking more than 4,000 mg daily for five or more years increases chronic kidney disease risk by 68%. That’s about 12 regular-strength pills a day. Many people hit that number without realizing it-combining cold meds, migraine pills, and pain relievers.
But the real danger? Combination products. Excedrin, Goody’s Powder, Midol, and others mix acetaminophen, aspirin, and caffeine. A 2018 meta-analysis found these are 3.7 times more likely to cause kidney damage than single-ingredient pills. Caffeine makes the kidneys work harder. Codeine adds more stress. And people don’t realize they’re taking multiple drugs at once.

Who’s at Highest Risk?
You’re at higher risk if you:
- Take NSAIDs or acetaminophen daily for more than 3 years
- Take 6 or more pills a day
- Have high blood pressure, diabetes, or existing kidney disease
- Are a woman over 30 managing chronic headaches or menstrual pain
- Use multiple OTC products at the same time
Women make up 72% of cases. Why? Many use these meds daily for conditions that aren’t taken seriously-migraines, endometriosis, fibromyalgia. They’re told “just take something,” and no one warns them about the kidneys.
And here’s the kicker: 62% of patients say they didn’t believe OTC painkillers could hurt their kidneys. That’s the real problem-not lack of drugs, but lack of awareness.
What Does the Science Say About Safer Options?
Good news: you don’t have to live in pain. There are safer ways.
Topical NSAIDs (gels, patches) are a game-changer. A 2021 study showed they relieve arthritis pain just as well as oral pills-but with 90% less drug entering your bloodstream. No kidney stress. No liver overload. Just apply it where it hurts.
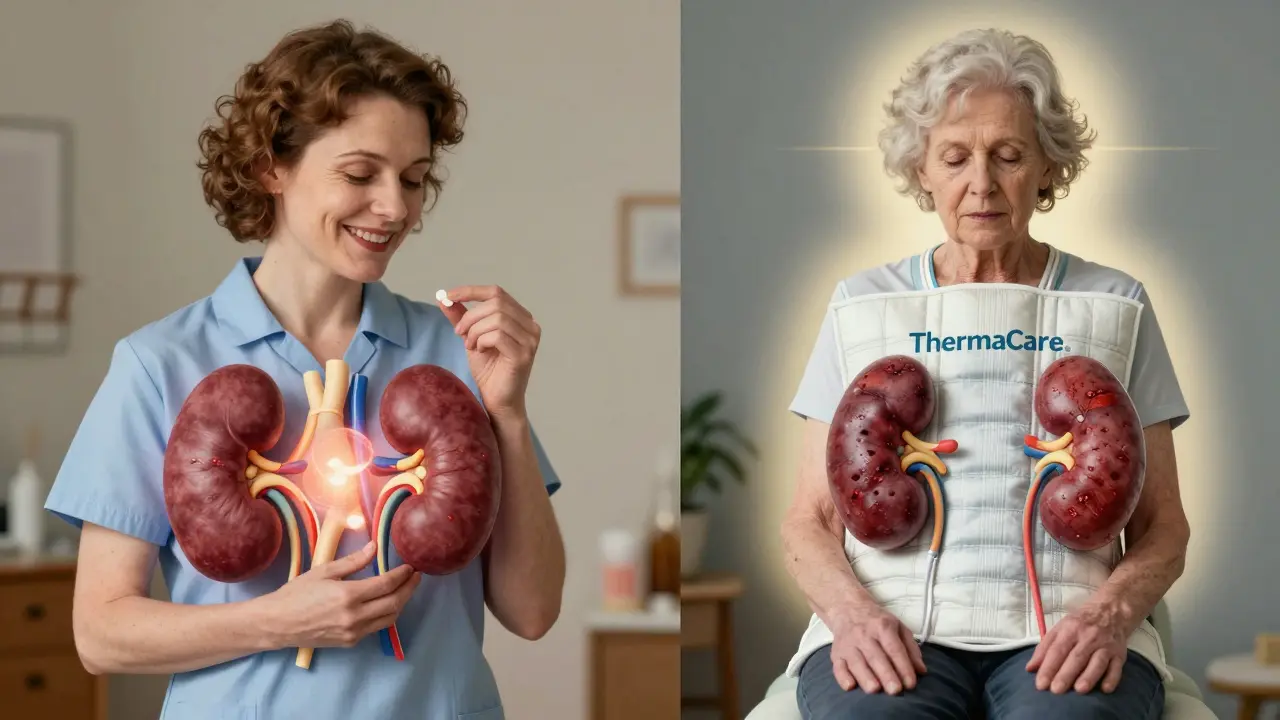
Heat therapy works better than you think. FDA-cleared heat wraps like ThermaCare reduce osteoarthritis pain by 40-60% without any drugs. Heat loosens stiff muscles, improves circulation, and reduces inflammation naturally.
Physical therapy and CBT are now recommended as first-line treatments. The American College of Rheumatology says: try non-drug options for 4-6 weeks before reaching for pills. Movement, stretching, and even talking to a therapist about pain coping strategies can cut pain by half.
Acetaminophen limits: Don’t exceed 3,000 mg per day. That’s six 500 mg tablets. And never mix it with other meds that contain it-cold and flu pills, sleep aids, prescription painkillers.
NSAID limits: No more than 1,200 mg ibuprofen or 750 mg naproxen per day for chronic use. And never take them for more than 10 days straight without checking with your doctor.
What Should You Do If You’ve Been Taking These Daily?
Step 1: Stop assuming they’re safe. Even “low-dose” daily use adds up.
Step 2: Get a simple blood test. Check your serum creatinine and estimated GFR (glomerular filtration rate). If your GFR is below 60 for more than 3 months, you have kidney disease.
Step 3: Talk to your doctor about switching. Ask for a topical NSAID, heat therapy, or referral to physical therapy. If you have migraines, ask about CGRP inhibitors-new prescription meds with no kidney risk, though they’re expensive.
Step 4: Monitor. If you must keep using painkillers, get your kidney function checked every 6 months. If you have diabetes or high blood pressure, check every 3 months.
Step 5: Track your intake. Use a journal or app. Write down every pill you take-even the ones you think don’t count. You’ll be shocked how fast the numbers add up.
What Happens If You Stop?
Here’s the hopeful part: if caught early, stopping the meds can stop the damage.
The 2022 study of 142 patients showed that 73% stabilized their kidney function after quitting analgesics. No dialysis. No transplant. Just stopping the pills and letting the kidneys heal.
One woman in her 50s, diagnosed with early-stage analgesic nephropathy after years of daily Excedrin, switched to heat wraps and physical therapy. Her GFR went from 58 to 68 in 18 months. She still has pain-but now it’s manageable, and her kidneys are stable.
But if you wait too long? Once scar tissue forms, it’s permanent. That’s why early detection matters more than you think.
Why Isn’t This Common Knowledge?
Because the pharmaceutical industry doesn’t advertise the risks. Because doctors assume patients know. Because OTC means “safe” to most people.
The FDA updated NSAID labels in 2020 to include kidney risk warnings. But they’re buried in fine print. Manufacturers like Bayer and Johnson & Johnson have reduced caffeine and acetaminophen in combo products-but they haven’t removed them entirely.
And here’s the truth: no one is teaching this in schools. No one is warning you when you buy a bottle of Advil. The burden falls on you.
So ask yourself: if your kidneys fail, will you wish you’d listened sooner?
Can I still take ibuprofen if I have high blood pressure?
If you have high blood pressure, NSAIDs like ibuprofen can make it worse and damage your kidneys faster. Avoid daily use. If you need pain relief, try topical NSAIDs, heat therapy, or acetaminophen (under 3,000 mg/day). Always check with your doctor before taking any painkiller if you have hypertension.
Is acetaminophen safe for kidneys?
Acetaminophen is less harmful to kidneys than NSAIDs-but it’s not risk-free. Taking more than 3,000 mg daily for years can still increase your risk of chronic kidney disease by 68%. Avoid daily use. Never combine it with other meds containing acetaminophen, like cold or sleep aids.
How do I know if my painkiller is harming my kidneys?
The only way to know is through blood tests. Ask your doctor for a serum creatinine test and estimated GFR. If your GFR is below 60 for more than 3 months, you have kidney disease. Early stages have no symptoms-so don’t wait for pain to appear.
Are there any new treatments for analgesic nephropathy?
There’s no cure for advanced damage, but early detection is improving. In January 2023, the FDA approved a new urine test called NephroCheck that detects early kidney damage with 92% accuracy. Research is also underway for kidney-sparing painkillers, but none are available yet. Right now, stopping the meds and protecting your kidneys is the best treatment.
Can I use CBD for pain instead of NSAIDs?
CBD products are popular, but their safety for kidneys isn’t well proven. A 2022 study found no kidney damage at doses under 1,500 mg/day, but long-term effects are unknown. They’re not regulated, so potency and purity vary. Don’t assume CBD is safe just because it’s natural. Talk to your doctor before switching.




Mandy Vodak-Marotta
February 2 2026I used to take 8 ibuprofen a day for my back pain-thought it was fine since it was 'over the counter.' Turned out my GFR was 52. No symptoms, no warning. Just a routine blood test. I switched to heat wraps and physical therapy. My kidneys are stable now, and I actually feel better overall. No more brain fog from the meds. Seriously, if you're on daily painkillers, get tested. It's not scary-it's just smart.