Diabetic retinopathy doesn’t come with warning signs. You might feel fine, see clearly, and think your diabetes is under control-until one day, your vision starts to blur, or you notice dark spots floating in your sight. By then, the damage is already done. This isn’t rare. About 1 in 3 adults with diabetes in the U.S. will develop some form of retinal damage from high blood sugar over time. And it’s the leading cause of vision loss in Americans between the ages of 21 and 64.
How High Blood Sugar Attacks Your Retina
Your retina is the light-sensitive layer at the back of your eye. It turns light into signals your brain reads as images. But when blood sugar stays high for years, it slowly damages the tiny blood vessels that feed the retina. These vessels become weak, leaky, or blocked. At first, you won’t notice anything. That’s the danger.The damage starts with microaneurysms-tiny bulges in vessel walls that leak fluid. Then, more vessels get blocked. Without enough blood flow, parts of the retina start to starve. In response, your eye tries to fix it by growing new blood vessels. But these new vessels are fragile. They bleed easily. They can pull on the retina and cause it to detach. They can also block fluid drainage in the eye, leading to a painful condition called neovascular glaucoma.
When fluid leaks into the macula-the center of the retina responsible for sharp, detailed vision-you get diabetic macular edema (DME). This is what causes blurry, wavy, or distorted vision. About 6.7% of people with diabetes develop DME. It’s not a separate disease-it’s a complication of diabetic retinopathy. And it’s one of the most common reasons people with diabetes lose their ability to read, drive, or recognize faces.
Three Stages of Retinal Damage
Diabetic retinopathy doesn’t happen overnight. It moves in stages:- Mild Nonproliferative Retinopathy: Small bulges (microaneurysms) form in retinal blood vessels. No symptoms yet.
- Moderate to Severe Nonproliferative Retinopathy: More vessels are blocked. The retina may swell, bleed, or show signs of oxygen deprivation. Vision might start to blur.
- Proliferative Diabetic Retinopathy: The eye grows new, abnormal blood vessels on the retina’s surface. These vessels bleed into the vitreous (the gel inside your eye), cause scar tissue, and can lead to retinal detachment. This stage carries a high risk of sudden, severe vision loss.
Diabetic macular edema can happen at any stage. You don’t have to reach the third stage to lose vision. That’s why waiting for symptoms is a mistake.
Why You Might Not Notice Anything Until It’s Too Late
Most people with early diabetic retinopathy have no symptoms. Not even a flicker of blur. Not even glare at night. A study from the University Health’s Texas Diabetes Institute found that 68% of patients didn’t notice vision changes until their retinopathy was already moderate or severe.By the time symptoms appear, the damage is often advanced. Common signs include:
- Floaters or dark spots that don’t go away
- Blurred or wavy vision, especially when reading
- Difficulty seeing in low light or at night
- Fading or washed-out colors
- Loss of peripheral vision
- Sudden vision loss from bleeding inside the eye
Many patients report their first symptom is difficulty driving at night. Others notice their vision fluctuates-clear one day, blurry the next. That’s often a sign of changing fluid levels in the retina. It’s not a fluke. It’s a red flag.
Laser Treatment: How It Stops the Damage
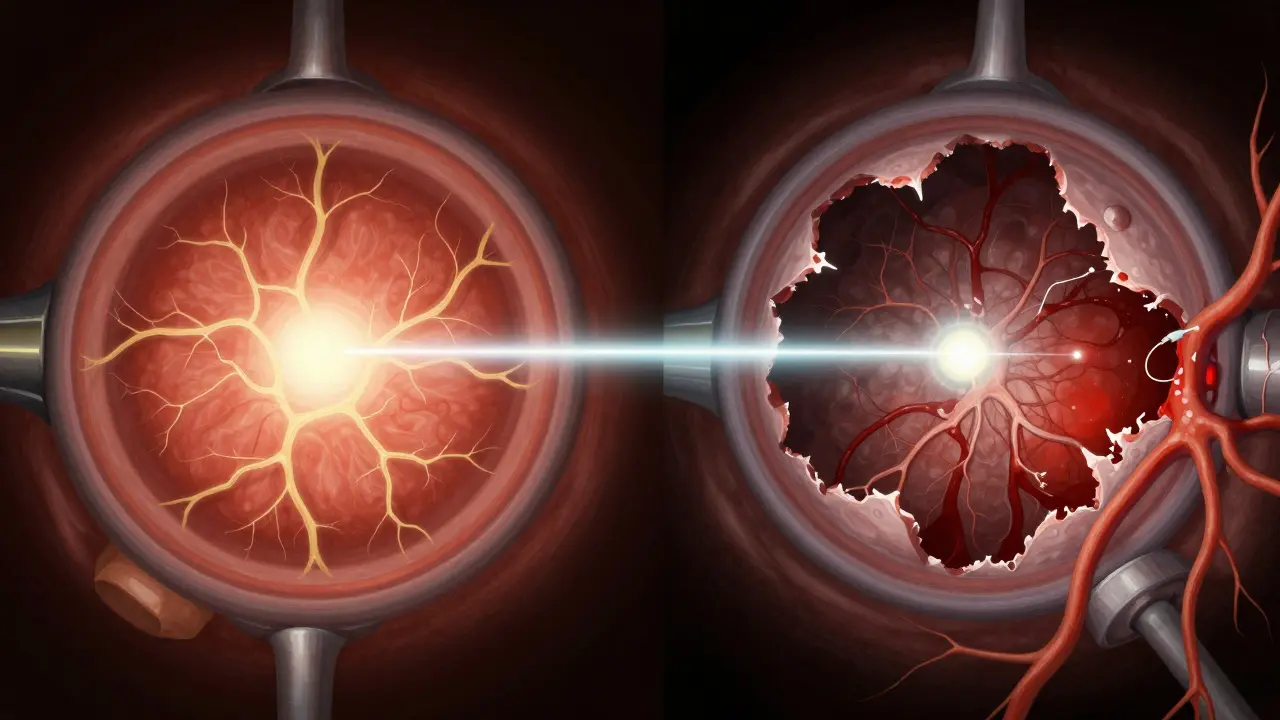
Laser treatment, called photocoagulation, has been the gold standard for treating advanced diabetic retinopathy for decades. It’s not a cure, but it can stop the disease from getting worse-and in many cases, save your vision.There are two main types of laser therapy:
- Focal/Grid Laser for Macular Edema: This targets specific leaky blood vessels near the macula. The laser seals them off, reducing swelling. It doesn’t restore lost vision, but it can prevent further blurring.
- Scatter (Panretinal) Laser for Proliferative Retinopathy: This treats the entire retina, not just one spot. The laser creates hundreds of tiny burns in the peripheral retina. This reduces the retina’s demand for oxygen, which tells the eye to stop growing those dangerous new blood vessels.
Think of it like cutting off fuel to a fire. The laser doesn’t remove the abnormal vessels-it starves them. Over weeks, they shrink and fade. Bleeding stops. Scar tissue doesn’t form as aggressively. The goal isn’t perfect vision-it’s preventing total vision loss.
Studies show that patients who get timely laser treatment have a 95% chance of preserving their current vision. That’s not a guarantee of 20/20 sight, but it means you won’t go blind. For someone who’s still working, driving, or caring for family, that’s everything.
Laser Isn’t the Only Option Anymore
In recent years, injections of anti-VEGF drugs-like ranibizumab (Lucentis) or aflibercept (Eylea)-have become common alternatives or complements to laser. These drugs block the protein (VEGF) that tells the eye to grow abnormal blood vessels. They’re injected directly into the eye, usually every few weeks or months.Anti-VEGF treatments are especially effective for diabetic macular edema. In many cases, they reduce swelling better than laser alone. Some patients get better vision after injections. Others get stability. But they require ongoing treatment. Laser, on the other hand, is often a one-time or limited procedure.
Today, many eye specialists use a combination approach: anti-VEGF injections to reduce swelling quickly, followed by laser to prevent future growth. The choice depends on your stage of disease, how much swelling you have, and how well your blood sugar is controlled.
What You Can Do to Prevent It
The best treatment for diabetic retinopathy is prevention. And the most powerful tool you have is control.Research from the Cleveland Clinic and others shows a direct link between your HbA1c levels (a measure of long-term blood sugar) and how fast retinopathy progresses. Every 1% drop in HbA1c reduces your risk of retinopathy progression by about 30%. That’s not a small number. It’s life-changing.
Here’s what works:
- Keep blood sugar steady. Avoid spikes and crashes. Use continuous glucose monitors if you can.
- Control blood pressure. High pressure adds stress to already damaged vessels. Aim for under 130/80.
- Manage cholesterol. High LDL contributes to vessel blockage.
- Don’t smoke. Smoking speeds up blood vessel damage throughout your body-including your eyes.
- Get annual eye exams. Even if you feel fine. Dilated eye exams are the only way to catch early damage.
For people with Type 1 diabetes, screening should start five years after diagnosis. For Type 2, it should begin right after diagnosis. Pregnant women with diabetes need an exam in the first trimester and possibly more during pregnancy-hormonal changes can make retinopathy worsen fast.
What Happens If You Ignore It?
Ignoring diabetic retinopathy doesn’t mean you’ll just get a little blurry vision. It means you risk permanent, irreversible blindness.Once photoreceptor cells-the light-sensing cells in your retina-die from lack of oxygen or pressure from bleeding, they don’t come back. No laser, no injection, no surgery can restore them. The damage is done.
And it’s not just your eyes. Diabetic retinopathy is a sign that blood vessels throughout your body are under stress. People with advanced retinopathy are at higher risk for kidney disease, nerve damage, and heart problems. Treating your eyes isn’t just about sight-it’s about your whole health.

Real Stories, Real Outcomes
One patient, a 52-year-old teacher with Type 2 diabetes, didn’t get an eye exam for seven years. She thought her glasses were just getting old. When she finally went in, she had severe proliferative retinopathy and macular edema. She got three anti-VEGF injections and a scatter laser treatment. Her vision didn’t improve-but it didn’t get worse. She kept her job. She kept driving.Another man, 45, with well-controlled diabetes, got his annual screening. His doctor spotted early microaneurysms. He tightened his diet, started exercising, and saw his HbA1c drop from 7.8% to 6.4%. Two years later, his retina was clear. No laser needed.
The difference? One waited until it hurt. The other acted before it started.
What to Expect During and After Laser Treatment
Laser treatment is done in the doctor’s office. You’ll get numbing drops. You won’t be asleep. The procedure takes 10 to 30 minutes. You might feel a brief stinging sensation with each laser pulse. It’s uncomfortable, but not unbearable.Afterward, your vision will be blurry for a few hours. You’ll need someone to drive you home. You might see floaters or spots for days. That’s normal. Your eye is healing.
Some people notice a slight loss of peripheral vision or night vision after scatter laser. That’s a trade-off. It’s better than losing central vision entirely. You’ll need follow-up visits every few months to make sure the treatment is holding.
Don’t expect miracles. Laser doesn’t restore lost vision. But it stops the train before it crashes.
Can diabetic retinopathy be reversed?
Early damage, like mild swelling or microaneurysms, can sometimes improve with strict blood sugar control and treatment. But once photoreceptor cells die or scar tissue forms, the damage is permanent. That’s why early detection is critical-treatment can stop progression, but it can’t undo what’s already gone.
How often should I get my eyes checked if I have diabetes?
If you have Type 1 diabetes, get your first eye exam within five years of diagnosis, then annually. If you have Type 2, get your first exam right after diagnosis, then yearly. If you have any signs of retinopathy, your eye doctor may recommend exams every 3 to 6 months. Pregnant women with diabetes need an exam in the first trimester and possibly more during pregnancy.
Does laser treatment hurt?
You’ll get numbing drops, so you won’t feel pain. You might feel pressure or a quick stinging sensation with each laser pulse. Most people describe it as uncomfortable, not painful. The whole procedure lasts less than half an hour.
Can I drive after laser treatment?
No, not right away. Your pupils will be dilated, and your vision will be blurry for several hours. You’ll need someone to drive you home. Avoid driving until your doctor says it’s safe.
Is laser treatment the only option for diabetic retinopathy?
No. Anti-VEGF injections are now commonly used, especially for diabetic macular edema. In some cases, they’re used before or instead of laser. Surgery may be needed if there’s a vitreous hemorrhage or retinal detachment. The best approach depends on your stage of disease, overall health, and how well your diabetes is controlled.
Next Steps: Don’t Wait for Symptoms
If you have diabetes, your next eye exam isn’t optional. It’s your best defense against blindness. Schedule it now. Don’t wait until you see floaters or your night vision gets worse. By then, it’s too late to reverse the damage.Take control. Lower your HbA1c. Control your blood pressure. Quit smoking. And get that dilated eye exam. Your eyes won’t tell you when they’re in trouble. But you can tell them-before it’s too late.



Sarah Mailloux
January 16 2026I had no idea diabetic retinopathy could sneak up like this. My mom had Type 2 and never got checked until she couldn't read her grandkids' birthday cards. She got laser treatment and still drives. Don't wait. Seriously.